Each year, 3 million people aged 65 years and over fall and 5 000 people die as result of the fall (National Institute for Health and Care Excellence (NICE), 2018; Age UK, 2019). Ageing increases the risk of falls and of sustaining an injury when a fall occurs. People aged 80 years and over are more likely to incur a fracture when they fall (NICE, 2018; Jennison and Brinsden, 2019). On average, 248 000 people in England are admitted to hospital annually because of fractures caused by falls (Jennison and Brinsden, 2019).
As people age, they are more likely to develop long-term conditions. In the UK, around 19 million people have long-term conditions (Office for National Statistics (ONS), 2020). When a person has two or more long-term health conditions, this is known as multimorbidity (NICE, 2016). The prevalence of comorbidities and multimorbidity is rising in line with population ageing and growing levels of ill-health and long-term conditions in younger people (Kingston et al, 2018). The latest data is reported to be less accurate than usual due to the impact of the COVID-19 pandemic (NHS Digital, 2022).
Increasing numbers of middle-aged and older people with multimorbidity have led to a dramatic rise in polypharmacy. In the last 20 years, the proportion of older people, those aged 65 years and over, taking five or more medications has quadrupled from 12 to 49% (Gao et al, 2018). Medicines can harm as well as heal and older people are more vulnerable to the adverse effects of medication, including drowsiness, increased risk of falls, increased risk of hospital admission and reduced quality of life. It is vital that medication is prescribed appropriately and reviewed to determine if it is still required. Unfortunately, this is not always the case, as the World Health Organization (WHO) (2022) comment:
‘Rational use of medicines requires that patients receive medications appropriate to their clinical needs, in doses that meet their own individual requirements, for an adequate period of time, and at the lowest cost to them and their community.
Irrational use of medicines is a major problem worldwide. WHO estimates that more than half of all medicines are prescribed, dispensed or sold inappropriately, and that half of all patients fail to take them correctly. The overuse, underuse or misuse of medicines results in wastage of scarce resources and widespread health hazards.’
This article aims to enable readers to understand why older people are at greater risk of adverse effects of medication, how polypharmacy increases those risks, what types of medication increase the risk of falls, the importance of medication reviews and how these are carried out.
How age-related changes increase the risk of adverse medication effects
Clinical trials are carried out before drugs are approved; however, people aged 65 or over are underrepresented in clinical trials. This means that the efficacy of a drug and the side effects noted may not be the same in older people and those from racial and ethnic minorities and low-income communities (Fisher et al, 2022).
Normally, drugs given orally are absorbed in the small intestine, metabolised in the liver and excreted by the kidneys (Garza et, al, 2022). Age-related changes cause reduced ability to absorb and excrete drugs. Ageing affects the rate of stomach emptying and the speed in which food and medicines travel through the gastrointestinal tract; blood flow is also reduced. This affects the absorption of medication (Dumic et al, 2019). As people age there is a decline in muscle mass and an increase in fat; this affects the way medicines are absorbed (Distefano and Goodpaster, 2018). The size of the liver reduces by 20% in older age and blood flow to the liver is reduced by 40%; these changes reduce the ability to metabolise drugs (Kim et al, 2015).
Many medicines are excreted from the body by the kidneys; however, renal function declines with age and this can impair the ability to excrete medication (Sönnerstam et. al, 2016).
Age-related changes at the molecular level can alter the way drugs bind to specific receptors. This can increase or decrease the effect of a medicine in an older person (Davies et al, 2020).
Age-related changes affect the way an older person's body reacts to medication and a medicine that was suitable for a person when younger may be inappropriate as they age. Older people and their families can find this difficult to understand and can resist changes to medication:
‘I don't understand why you want to cut down mum's sleeping pills. They can't be causing falls…she's been taking them for 40 years’
The older women is now 40-years-older and age-related changes have affected her ability to metabolise the medication.
Age-related changes affect the risk of a person suffering adverse drug reactions (ADRs). ADRs are:
‘…unintended, harmful events attributed to the use of medicines.’
(Coleman and Pontefract, 2016)
ADRs can have a major effect on a person's health and quality of life.
How polypharmacy affects the risk of falls
There is no universal definition of polypharmacy. It might be better to consider the appropriateness of the medications, rather than the number. The WHO (2019) defines polypharmacy as:
‘…the concurrent use of multiple medications. Although there is no standard definition, polypharmacy is often defined as the routine use of five or more medications. This includes over-the-counter, prescription and/or traditional and complementary medicines used by a patient.’
The most common definition of polypharmacy is five or more medications. However, few articles have distinguished between appropriate and inappropriate polypharmacy (Masnoon et al, 2017). It is important to determine the risks and benefits of medicines and if the person is willing and able to comply (Parsons, 2017). One inappropriate medicine can adversely affect a person's life while a number of appropriately prescribed medicines can improve a person's life.
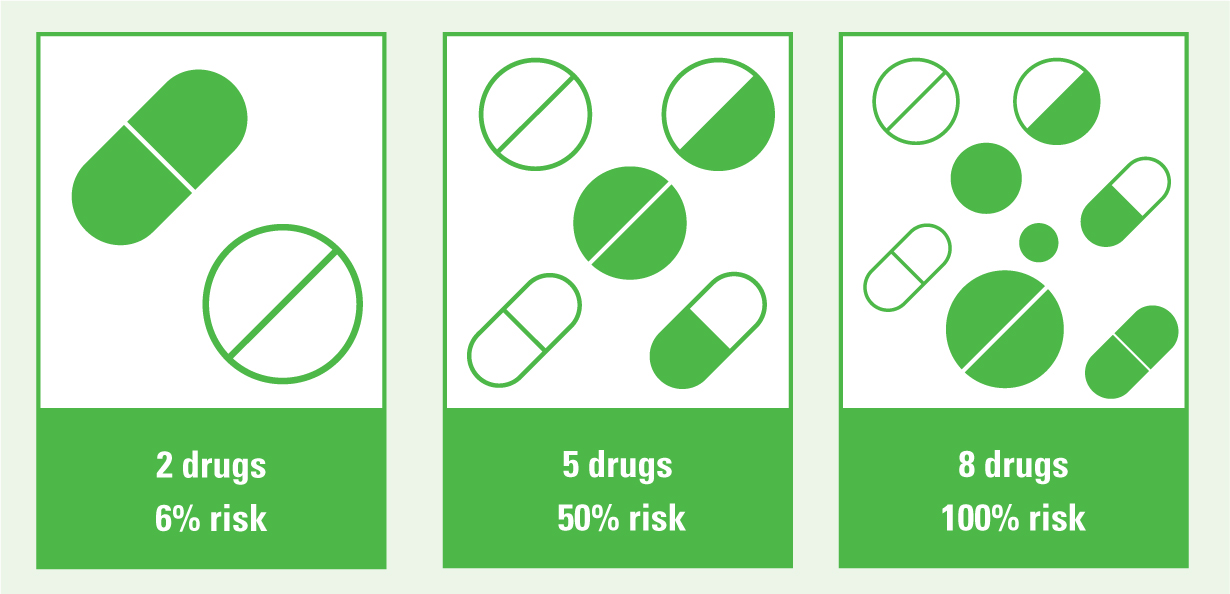
Polypharmacy increases the risk of falls. The greater the number of medicines a person takes, the greater the risk that they will interact and the person will experience ADRs. Research indicates that the probability of ADRs among older people is estimated at 6% when two drugs are taken, increases to 50% when five drugs are taken, and becomes 100% when eight or more drugs are taken (Chumney and Robinson, 2006). This is illustrated in Figure one.
Adverse drug reactions lead to 5 700 deaths and cost £750 million to treat annually (Maidment et al, 2017). The number of people admitted to hospital because of ADRs is increasing; between 2007and 2015, the emergency admissions due to ADRs increased by 53.4%, and the number of bed days that were used due to ADRs also increased by 51.5% (Veeren and Weiss, 2017). Around 5–10% of older people who are admitted to hospital are a result of ADRs (Budnitz et. al, 2011; Oscanoa et al, 2017) Those ADRs can lead to falls, injury and hospital admission.
Cholinergic burden
Older people are often prescribed medicines with anti-cholinergic properties. They all work by blocking the action of acetylcholine, a type of neurotransmitter. Neurotransmitters are chemical messengers in the brain and blocking them inhibits involuntary muscle movements and various bodily functions. Medications with anticholinergic effects include medication to treat Parkinson's disease, hypertension, abnormal heart rhythms, depression, bladder problems and chronic obstructive pulmonary disease (Arthur et. al, 2020).
Case history
Paula Harris a 77 year old lady had two falls.
She slipped down the stairs at home whilst wearing unsuitable foot wear. She sustained heavy bruising to her back, attended hospital and was admitted for a few days. A month later she woke in the middle of the night needing to pass urine urgently. She slipped, fell and hit her cheekbone. Her eye was so bruised and swollen she couldn't open it. She again attended accident and emergency, x-rays showed that she had not fractured her orbit as initially suspected.
Careful history taking revealed that Paula had slipped on the stair carpet as she wasn't wearing her slippers. Her feet have become very swollen recently. She reported that her bladder has been “playing up” recently. She is now passing urine more frequently and having to get up in the night to pass urine. Medication review showed that Paula had been prescribed verapamil to treat high blood pressure and these are recognised side effects (EMC, 2023).
Blood pressure was well controlled so verapamil was discontinued and blood pressure carefully monitored. The symptoms that had led to falls, peripheral oedema, polyuria and nocturia resolved. Unfortunately, Paula's blood pressure crept up. She was prescribed another medication, bisoprolol 1.25mg for her blood pressure. This controlled blood pressure and Paula did not experience any adverse effects. She commented: ‘I've got my life back. That medicine aged me 10 years, I was exhausted getting up every night’.
It is now accepted practice that anticholinergic medications should be avoided whenever possible in older people (Gray et al, 2015). A recent study found that not only are they widely prescribed but their use in older people has nearly doubled in the last 20 years; those who are most vulnerable to adverse effects had the greatest increase in use (Grossi et al, 2020).
Older people prescribed anti-cholinergics frequently suffer adverse effects such as dry mouth, nausea, dizziness, fatigue, vomiting, constipation, abdominal pain, urinary retention, blurred vision, tachycardia and neurologic impairment such as confusion and agitation (Fox et al, 2011). Anticholinergic medication can cause daytime drowsiness, cognitive decline and increase the risk of falls (Richardson et al, 2015). They can increase the risk of institutionalisation and lead to increased mortality (Collamati et al, 2016). A third to half of all medications prescribed for older people have anticholinergic activity (Nishtala et al, 2016).
The number of anticholinergic medications used adds up to what is known as the ‘cholinergic burden’. High levels of cholinergic burden are associated with an increased risk of dementia and mortality (Gray et al, 2015; Coupland et al, 2019).
Minimising anticholinergic burden will improve short-term memory, minimise the risks of confusion and delirium and improve quality of life and daily functioning (Collamati et al, 2016). The healthcare professional can work out the cholinergic burden of medication using the Anticholinergic Cognitive Burden tool (https://www.acbcalc.com/).
What type of medications increase the risk of falls?
Any medicine that causes drowsiness, dizziness, confusion or slows reactions increases the risk of falls. Sleeping tablets, for example, are not recommended for long-term use and must be given with great care in older people; yet, many older people are prescribed them. These tablets increase the risk of falls and fractures (Andrade, 2018). Medicines known to cause drowsiness and confusion and increase the risk of falls and fractures include hypnotics such as zopiclone (Ryba and Rainess, 2020).
Antidepressant use is associated with recurrent falls (Marcum et al, 2016; Jung et al, 2022). Antidepressants such as fluoxetine can cause sedation, insomnia and impaired sleep. They can also cause nocturia, hypotension, cardiac rhythm and conduction disorders, and impair reaction times (Darowski et al, 2009).
Other medicines prescribed to treat conditions such as heart failure and high blood pressure can cause postural hypotension, which can increase the risk of falls.
Opioids such as codeine, morphine and oxycodone and nonsteroidal anti-inflammatory drugs (NSAIDS) such as diclofenac increase the risk of falls and fracture. The risks are lower with NSAIDS but both categories of medication increase the risk of kidney damage (Herzig et al, 2021).
Table 1. Medicines that increase the risk of falls
| Type medicine | Used for | Risk of falling | Reasons why |
|---|---|---|---|
| Diuretics | Hypertension, heart failure, fluid retention | High | Postural hypotension, dehydration |
| Beta blockers | Hypertension | High | Postural hypotension |
| Vasodilators | Hypertension | High | Postural hypotension |
| Alpha-blockers | Hypertension, difficulty with bladder emptying | High | Postural hypotension |
| Nitrates | Angina | High | Postural hypotension |
| Calcium channel blockers | Hypertension | High | Postural hypotension; Dizziness |
| Sedating antihistamines | Itching, cold and flu remedies | High | Drowsiness |
| Hypnotics | Insomnia | High | Daytime drowsiness |
| Antipsychotics | Severe anxiety often prescribed for agitation | High | Drowsiness, hypotension, increased stroke risk, cardiac arrhythmias |
| Tricyclic antidepressants | Depression | High | Drowsiness, cardiac arrhythmia |
| Opioid analgesics, strong painkillers | Moderate to severe pain | High | Drowsiness, confusion |
| Dopamine drugs | Parkinson's | High | Dizziness, vertigo |
| Digoxin | Heart failure | Medium | Confusion, low pulse if dose too high |
| ACE inhibitors | Hypertension | Medium/high | Rapid drop in blood pressure, dizziness |
| Laxatives | Constipation | Low | Dehydration, electrolyte imbalance, dizziness |
Medication review to address inappropriate prescribing
There are many definitions of potentially inappropriate prescribing. The common theme is that the risks of harm from a particular medication outweighs the benefits. O'Mahony and Gallagher (2008) define potentially inappropriate prescribing (PIP) as:
‘…using medicines that may cause more harm than benefit, are not cost-effective, or are not clinically indicated.’
Some medications such as hypnotics (sleeping tablets) should generally be avoided in older populations and in some cases, older people require smaller doses because of age-related changes (Cahir et al, 2010)
A review of medication prescribed in primary care found that 20% of medicines prescribed to older people were inappropriate (Opondo et al, 2012). A Swedish study of 813 older people attending primary care or a specialist healthcare setting found that 46% had one or more PIP. People with PIP had double the incidence of ADRs and 62.5% of the ADRs resulted in falls (Hedna et al, 2015).
PIP increases the risk of adverse drug reactions, accident and emergency attendance and hospital admission (Liew et al, 2019).
Medication reviews aim to ensure that the person is prescribed appropriate medication and promotes quality of life. Figure two illustrates this.

Who can carry out a medication review?
Medication reviews can be carried out by a range of healthcare professionals, including nurses and pharmacists who have completed specialist training to enable them to prescribe and review medication (Weeks et al, 2016).
Total NHS spending on medicines in England has risen from £13 billion in 2010–2011, to £18.2 billion in 2017–2018. This is an average growth of around 5% a year with 1.1 billion prescription items dispensed in primary care by GPs and pharmacists (Department of Health and Social Care, 2018). Medication reviews are essential to ensure that older adults are prescribed appropriate medications and are not at risk of ADRs including falls, that can have a major impact on their quality of life.
‘Most physicians continue to prescribe to the elderly medicines which should not be given at all, or not combined. Polypharmacy is a complex issue in old age, and in many cases treating physicians are not conducting critical assessment of the need for numerous medications.’
Physicians and pharmacists working in general practice report that they lack time to review medications and find it difficult to engage with patients (Duncan et al, 2019). Physicians may also be reluctant to change medication prescribed in hospital as they perceive this as being prescribed by a consultant.
As medicine becomes ever more specialised, primary care physicians may feel deskilled and defer to specialists;
‘I can't review the furosemide, it was prescribed by a cardiologist.’
The reality may be that the furosemide was prescribed inappropriately by a junior doctor for oedema, secondary to venous insufficiency. Non-medical prescribers such as nurses and pharmacists who specialise in caring for older people and other specialist areas such as diabetes or heart failure might be able to make a major contribution in this area.
What types of tools are available?
In the UK the Screening Tool Of Older People's Prescriptions (STOPP), Screening Tool to Alert to Right Treatment (START) is often used. This tool is based on literature review and the expertise of members from 13 European countries. This tool aims to alert prescribers to medications that are inappropriate (STOPP) and has a screening tool to alert to right treatment (START). It has 114 criteria: 80 STOPP criteria and 34 START criteria. The authors state that all drugs should be clinically indicated and set out broad criterion for discontinuation (Table 2).
Table 2. STOPP/START broad criterion for discontinuation of medication
| Any drug prescribed without an evidence-based clinical indication. |
|---|
| Any drug prescribed beyond the recommended duration, where treatment duration is well defined. |
| Any duplicate drug class prescription e.g. two concurrent NSAIDs, SSRIs, loop diuretics, ACE inhibitors, anticoagulants (optimisation of monotherapy within a single drug class should be observed prior to considering a new agent). |
A new version of the tool the ‘STOPP frail version 2’ was introduced to provide clinicians with a practical, patient-centred and, where possible, an up-to-date evidence-based approach to deprescribing decisions in older people approaching end-of-life. This aims to promote quality of life in older people who are in the last year of life (Curtin et. al, 2021).
The American Geriatrics Society Beers Criteria® is an explicit list of medications that are typically best avoided by older adults in most circumstances or under specific situations, such as in certain diseases or conditions. It is produced by the American Geriatrics Society and updated every three years (By the 2023 American Geriatrics Society Beers Criteria®Update Expert Panel, 2023).
Alternatives to medication
Prescribers do not prescribe in isolation; they generally prescribe in relation to an expressed need or problem. There is a perception in society that there is a pill for every ill. There often is, but those pills can sometimes have devastating side-effects on a person's life. Prescribers can and should consider alternative strategies to promote well-being. The prescriber can advise on sleep hygiene to promote sleep rather than prescribe medication (Age UK, 2022).
Case history
Margaret Hamilton was devastated when she lost David, her husband of 45 years. They had planned to travel and enjoy life. David had a heart attack and died suddenly. Margaret was heartbroken and was not eating or sleeping properly. Her GP referred her to CRUSE, a charity that supports bereaved people and offers counselling. This helped Margaret to deal with her grief and medication was not required.
Conclusion
There are many reasons why fall and medication review alone is not effective (Seppala et al, 2022). It should be part of a holistic review. Although people are aware of the hazards of polypharmacy and how it can increase the risk of falls, the number of potentially injurious medications prescribed to older people is rising. We need to improve our care of older people and remember to treat the whole person. Holistic care can make a huge difference to an older person's quality of life.
Key points
- The number of older people taking five or more medications has quadrupled in the last 20 years
- Older people are more vulnerable to adverse effects of medication due to age-related changes
- Polypharmacy increases the risk of drug interactions and falls
- Medication reviews are not always carried out when clinically indicated
CPD reflective questions
- Mr Michael Johnstone tells you he is constipated and asks if he can have something to help. What alternatives could you suggest?
- How could you, as a community nurse, work with GP practices to review medication in frail older people?
- How can nurses working in primary care work with colleagues and older people to review medications?


