Care staff in the care home sector make an invaluable contribution to older residents' care. However, many staff feel undervalued, and support for their training and development varies (Spilsbury et al, 2015). The NHS should support care homes, as emphasised by a Care Quality Commission (CQC) report which highlighted that over 40% of care homes in England either require improvement or are inadequate (CQC, 2016).
Locally, within the Thurrock area of Essex where the project lead (SL) works, care home residents have multiple hospital attendances and admissions. Smith et al (2015) reported that older people living in a care home postcode had 40–50% more emergency department attendances and emergency admissions than the general population of the same age. Nationally, a proactive strategy is needed to prevent deterioration of care home residents (Cavendish, 2013).
NICE has produced guidance for managing the care of older adults in care homes (NICE, 2015a). This addresses the prevention of deterioration by focusing on the following key areas: managing nutrition, preventing falls, reducing infections, avoiding delirium, monitoring for depression and supporting those with dementia. Adherence to this guidance should help prevent avoidable hospital admissions, but key to this is training and support for care staff. If the NHS is committed to continuous quality improvement, it is essential that healthcare workers are valued as a strategic resource. Locally, the Thurrock Clinical Commissioning Group is working to deliver care to older people living in their own homes and care homes, and to avoid unnecessary hospital admissions. Early detection of deterioration in older people living in care homes is a proposed strategy to improve care, so that these residents can be managed proactively. Early warning trigger tools are used nationally in acute hospitals to facilitate identification of deterioration, and these have proven beneficial (McArthur-Rouse, 2001; Burch et al, 2008; Smith et al, 2014; Roney et al, 2015). However, there is limited evidence of the efficacy of early warning tools in community settings, and to our knowledge, there was no early warning tool specifically for use in care homes for older adults at the time of this project.
The present study aimed to introduce an early warning tool, the Significant 7, to facilitate identification and management of deterioration in older adults living in a care home. The objectives were to increase staff confidence around recognising signs of potential resident deterioration, reduce the incidence of falls by 10% within 3 months and reduce the incidence of pressure ulcers by 10% within 3 months.
Methods
Context
One care home was recruited for the project (May 2016 to December 2016), and one residential unit within the home was initially selected (Table 1). SL had worked with this care home in her capacity as a nurse specialist for older adults and had established good working relationships with staff.
|
|
|
|
|
|
Stakeholder engagement and problem analysis
To understand the current process followed when residents deteriorated, a process map was completed. Process mapping enables a stakeholder group to identify current activity and areas for improvement (McLaughlin et al, 2014) and aims to maximise clinical efficacy and efficiency by removing unnecessary and ineffective steps (Trebble et al, 2010). The stakeholder group comprised the care home deputy manager, three senior carers, and five carers. The process was led by SL and two quality improvement practitioners from the community trust. This activity enabled stakeholders to gain insights into all stages of the process by determining how the process of identification and management of resident deterioration usually flows and by identifying any bottlenecks to inform the improvement process.
One such bottleneck was care staff knowledge about identifying resident deterioration. It was reported that some care staff recorded resident observations such as blood pressure and temperature while others did not. Interpretation of observations was also variable, for example, some care staff recorded observations but lacked knowledge of parameters. A second bottleneck was a lack of clarity about action to take when resident deterioration was identified. Residents who were unwell usually received a urine dipstick test, and if it yielded positive results, antibiotics were usually prescribed via the telephone. It was discussed that not all differentials were explored, and care staff were concerned that the information they conveyed over the telephone influenced the diagnosis if a general practitioner or nurse did not visit the resident. The information generated by process mapping informed the development of a driver diagram, a tool that provides an overall vision of the project including the aim, objectives and measures (ACT Academy NHS Improvement, 2017).
Measures
The measures for evaluating processes and impact are presented in Table 2. These included outcome, process and balancing measures.
| Outcome measures | Process measures | Balancing measures |
|---|---|---|
| Increase staff confidence |
Complete process mapping |
Ambulance callouts |
Behaviour change intervention
Process mapping identified that staff views varied about how to identify and manage deteriorating residents. Two staff members said that they were confident about this and did not require additional training; the other eight staff members welcomed the proposal for training and support. The success of any quality improvement project relies on successful behaviour change intervention(s), that is, coordinated activities designed to change the specified behaviour pattern (Michie et al, 2014). In this project, the COM-B model (Michie et al, 2014) was used by the project team to review capabilities, motivation and opportunities, and to inform the interventions.
Intervention
The intervention comprised the introduction of the Significant 7 early warning tool and a training programme about recognising deterioration. The Significant 7 tool and training were developed by North East London Foundation Trust and Barking and Dagenham, Havering and Redbridge Clinical Commissioning Groups. The tool addresses seven signs of deterioration—confusion, mood, pain, hydration, skin, breathing and toilet or bowel habits—and includes guidance on how to manage these signs.
To maximise staff engagement and attendance, multiple training dates were set. Each training session was treated as an individual plan, do, study, act (PDSA) cycle so that training content and implementation of the tool could be tailored accordingly.
PDSA cycle 1: 28.7.2016
PDSA cycle 2: 5.8.2016
| Training programme content |
|---|
|
|
For scenario (1), participants were given a checklist of the seven signs of deterioration. They were asked to work in pairs, where one person role played the resident while the other role played the carer. Facilitated by SL, a group discussion followed about the scenario and the signs of deterioration that were identified. A decision tree was introduced before scenario (2); the decision tree gives guidance to care staff on measures to take for each of the Significant 7 signs of resident deterioration.
For scenario (2), participants again worked in pairs using the roleplay cards. They used the checklist and the decision tree to ascertain what was wrong with the resident. The pairs were then asked to provide feedback to the whole group. Similarly, for scenario (3), participants worked in pairs and used the decision tree and the checklist. The weekly chart was introduced; this document allows care staff to record over a period of several days any resident problems identified for each of the Significant 7 signs. Each staff member who completed the training identified a resident for whom they could use the weekly chart. A date for the following week was set to meet care staff and review how they had got on using this.
The post-training questionnaire was completed immediately on completion of the training and again at 6 weeks after training.
PDSA cycle 3: 13.9.2016
PDSA cycle 4: 17.10.16
Data collection
Staff confidence
A staff questionnaire was administered at three time points: before training, immediately after training and 6 weeks after training. This questionnaire was prepared by the developers of the Significant 7 tool (North East London Foundation Trust and Barking and Dagenham, Havering and Redbridge Clinical Commissioning Groups). The pre-training questionnaire comprised five items that asked about the length of time spent working in this care home, the total length of time as a care worker, enjoying the job, finding the job rewarding and feeling confident to recognise when a resident is becoming unwell. The last three items were rated on a 5-point scale (1=strongly agree; 5=strongly agree).
The questionnaire administered immediately after training comprised six items that asked staff if they had enjoyed the training (rated on a 5-point scale where 1=strongly disagree and 5=strongly agree), if they had found the training useful (rated on a 5-point scale where 1=strongly disagree and 5=strongly agree), if they will use the training in their daily practice (rated on a 5-point scale where 1=strongly disagree and 5=strongly agree), how they think the training will change their practice (free text response), how they think the training could be improved (free text response) and if they would recommend the training to a colleague (yes/no response). The questionnaire administered 6 weeks after training comprised seven items that asked about enjoying the job, finding the job rewarding, feeling confident to recognise when a resident is becoming unwell, their use of the Significant 7 tool to identify changes in residents' health, their use of the decision tree, their use of the Handover Board and how the training has changed their practice for the better.
Incidence of falls and pressure ulcers
Baseline data were collected on the number of falls and pressure ulcers among the 22 residents in the participating residential unit. These data were collected from January 2016 onward (still underway).
Admissions to hospital and ambulance attendances
A request was made to the local hospital for admission data pertaining to the care home for the period of January to September 2016 and to the East of England Ambulance Service for ambulance attendance data.
Ethics considerations
The project was discussed with North East London Foundation Trust's Research and Development Office; ethics approval was not required as it was a quality improvement project. It was advised that if the results were not in keeping with good practice, this process would be reviewed.
Results
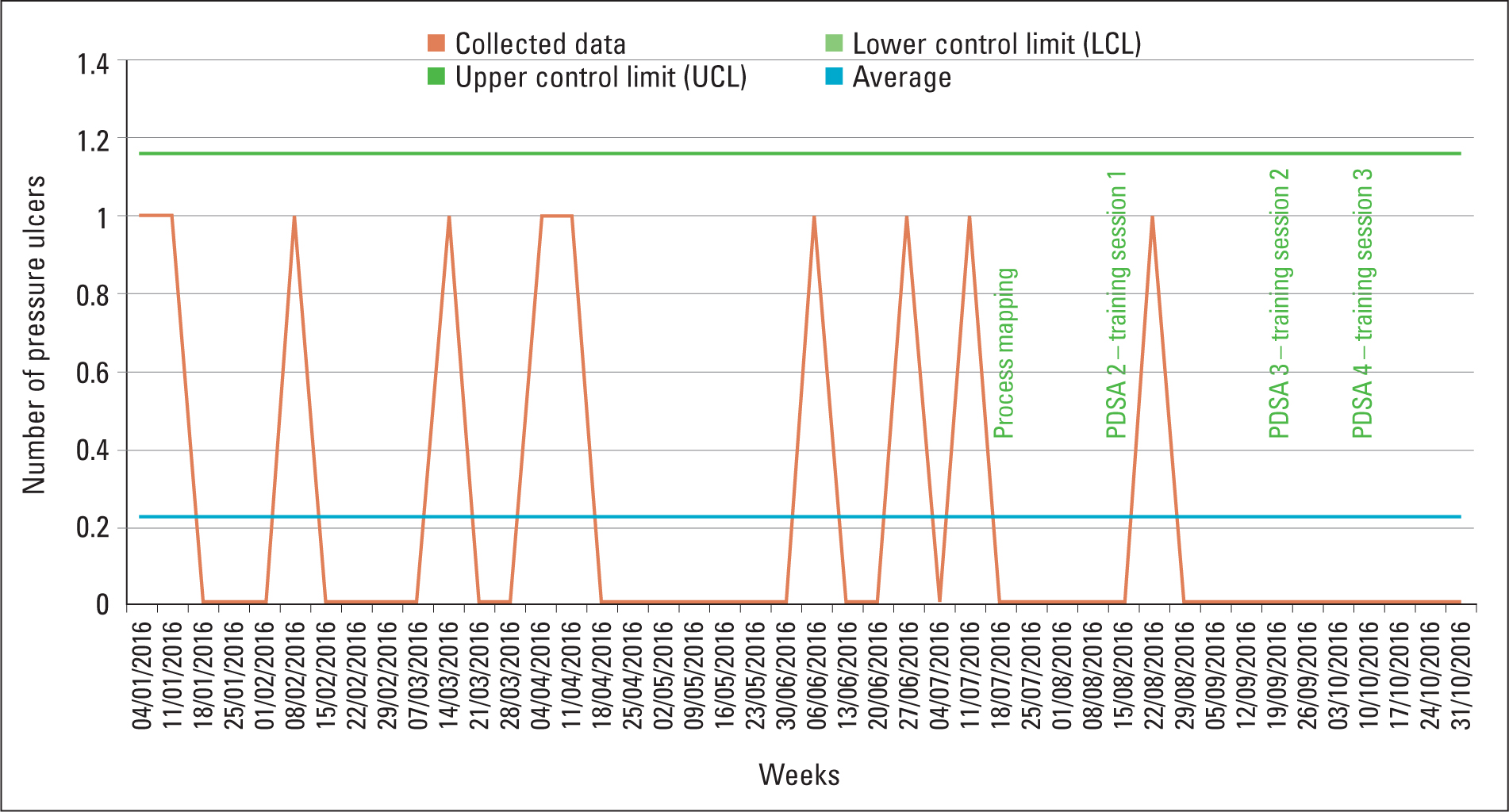
Incidence of pressure ulcers
The incidence of pressure ulcers among residents in the participating residential unit was measured before and after the intervention (Figure 1). The data show a reduction in the number of pressure ulcers after the intervention; before the intervention, eight pressure ulcers were recorded, while only one was recorded after the intervention.
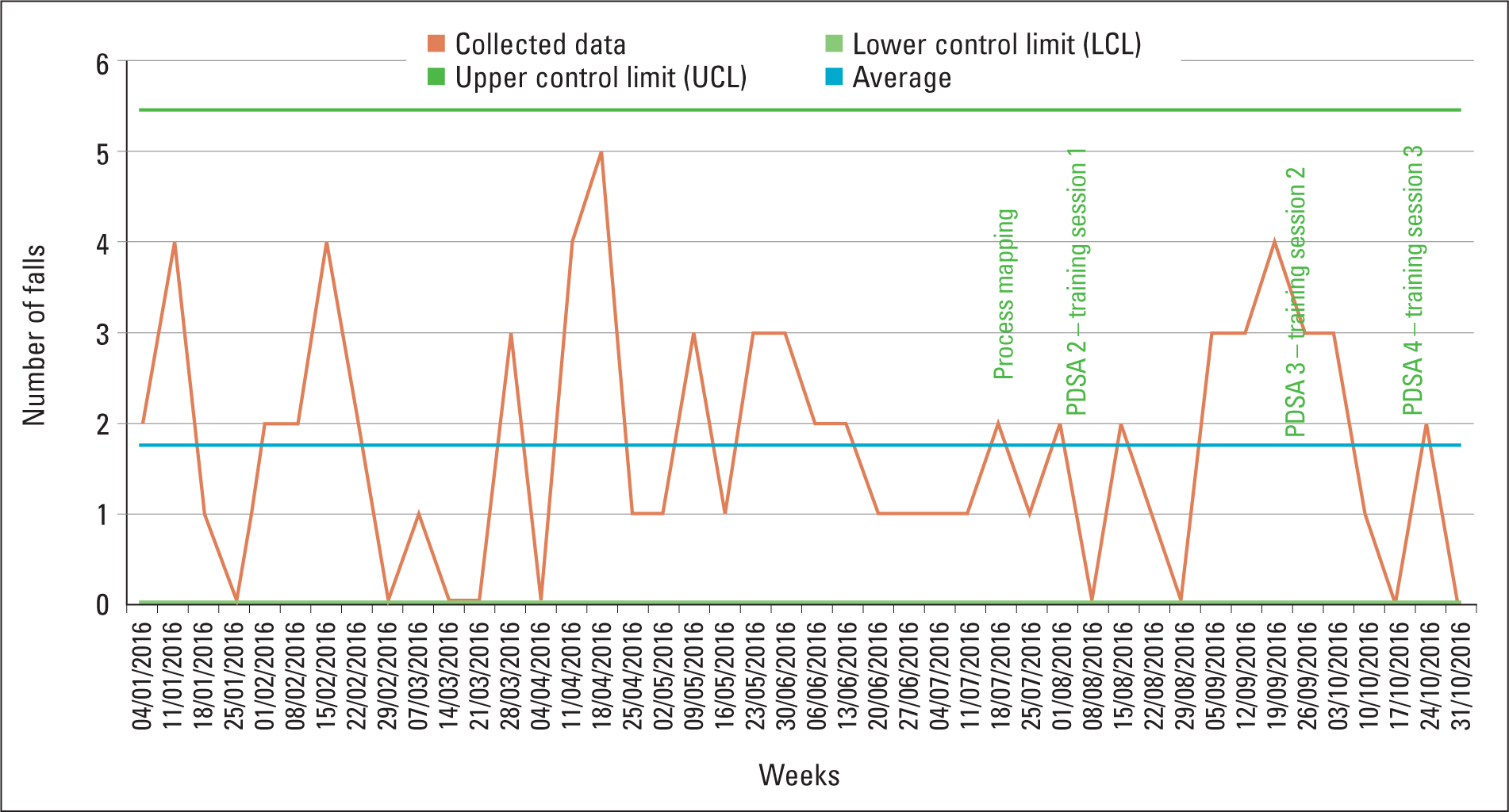
Incidence of falls
The number of falls in the participating residential unit was also measured before and after the intervention (Figure 2). The data indicated an overall reduction in the incidence of falls. A peak in the number of falls was observed between 5 September 2016 and 10 October 2016, and further analysis of the data revealed that one resident had had multiple falls in this period. Excluding this peak, only six falls were recorded after the intervention.
Staff confidence
Fifteen staff members completed the pre- and immediately post-training questionnaires. To date, eight staff members have completed the 6-week post-training questionnaire.
According to the pre-training questionnaire, most staff members strongly agreed or agreed that they enjoyed their job, although for each training session, four staff members neither agreed nor disagreed. There was a variation in the answers received for the statement ‘I find my job rewarding’: two staff members strongly agreed, 11 agreed, one neither agreed or disagreed and one disagreed. Similarly, two members strongly agreed to feeling confident about recognising when residents become unwell, 11 agreed and two neither agreed nor disagreed.
According to the post-training findings, all 15 staff members agreed or strongly agreed that they enjoyed the training, found it useful, would use the training in their practice and would recommend it to a colleague. There were no recommendations for improvement, suggesting that the participants were satisfied with the training they received. Examples of participant feedback about how the training would change their practice are presented in Figure 3.
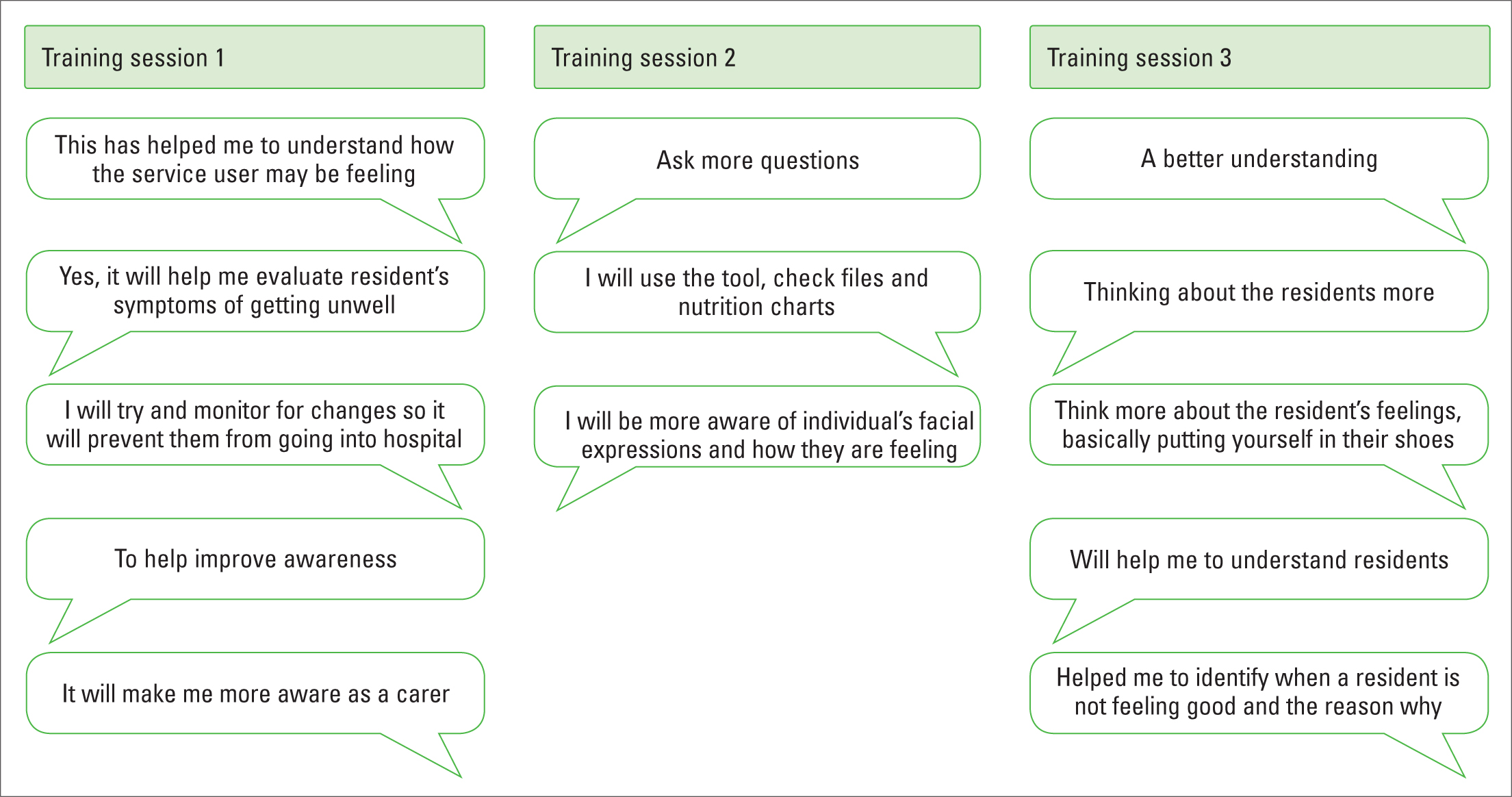
At the time of writing, 6 weeks had elapsed since completion of training for two of the three groups. For these two groups, all 15 staff members either agreed or strongly agreed that they enjoyed their job and found their job rewarding. This was an improvement from the pre-training questionnaire. All participating staff members agreed or strongly agreed that the training had changed their practice for the better, and 12 strongly agreed and three agreed that they felt confident that they could recognise deterioration. Twelve reported using the Significant 7 tool daily and three reported using it at least weekly. Ten reported using the decision tree daily and five used it at least weekly. Lastly, 14 reported using the Handover Board daily and one used it at least weekly.
Rates of hospital admission and ambulance attendance
The data for admissions to the local hospital and ambulance attendance were not resident specific and could not be separated out for the participating residential unit. The project team will continue to collect these data to evaluate the impact of Significant 7 training once it has been implemented for the entire care home.
Discussion
The prevention of pressure ulcers is an important NHS goal (Department of Health, 2011; NICE, 2015b). The project care home was completing Safety Cross and completing risk assessments for residents, and baseline data indicated that the overall incidence of pressure ulcers was low. Zero tolerance to pressure ulcers is at the core of the Stop the Pressure NHS Improvement Campaign (nhs.stopthepressure.co.uk), and a project objective was therefore to reduce the incidence of pressure ulcers by 10% within 3 months. The results show that this objective was achieved, with a 23% decrease in pressure ulcers over a 3-month period. Horn et al's pilot study (2010) to investigate pressure ulcer prevention in long-term care settings reported a reduction in the incidence of pressure ulcers where there was evidence of strong multidisciplinary commitment to changing attitudes. During our project as well, it became evident early on that investing time with care staff was critical to help maximise staff motivation to embrace change (Michie et al, 2014).
Falls are a common problem for older adults, leading to injury, dependency and death (Dyer et al, 2004; NICE, 2013). Thus, a project objective was to reduce falls by 10% within 3 months of training completion, and the results demonstrated a reduction. Analysis identified a peak in the falls rate between 5 September 2016 and 3 October 2016, and further analysis showed that this was attributable to one resident who was falling repeatedly and was subsequently admitted to hospital due to falls. A falls care plan was in place for this resident as well as a strategy for the care home to reduce or eliminate falls. Data collection for the incidence of falls is ongoing to enable further analysis.
The success of any quality improvement project involving staff members relies on their willingness to engage and commit to behaviour change. Using the COM-B model allowed for opportunities, motivation and capabilities to be examined and acted upon (Michie et al, 2014). The questionnaire data showed that all staff trained (n=15) now feel confident about recognising signs of resident deterioration. The number of staff members who enjoy their job and those who find their job rewarding also increased after the intervention. Castle et al (2007) suggested that low job satisfaction is associated with high staff turnover. Further, Edvardsson et al (2011) investigated job satisfaction among care staff and found that supporting care staff to provide person-centred care was correlated with job satisfaction and reduced turnover. Training to support implementation of the Significant 7 tool aimed at promoting individualised resident-centred care, which may explain the improvements observed.
Project strengths and limitations
The PDSA method allowed for continuous improvements to the intervention, and process mapping facilitated early engagement with the care home staff. Early engagement allows for staff to share the project vision, fostering a sense of ownership and motivation (Michie et al, 2014). It may have been beneficial to have conducted stakeholder focus groups, as not all care staff were involved in the process mapping.
From our previous experience working with this care home, we observed that the organisation and staff were receptive to new ideas. For this project, staff were under no obligation to comply with either the training or the use of the Significant 7 tool. The leadership styles of the care home manager, unit manager and the project lead were influencing factors for the success of the project. This stage of the project involved only one unit within the participating care home, which should be borne in mind when considering the findings. Unfortunately, data for acute hospital admission and ambulance attendance were not resident or unit specific, which prevented their inclusion in the analysis; these data will be examined in future work.
Conclusion
This project has shown that implementation of an early warning tool with a training programme can have positive effects on the identification and management of deterioration in older adults living in care homes. The next stage is to deliver the intervention in the remaining three units of the care home to further inform the process of improvement and a strategy for sustainability of improvement. This includes being able to offer this intervention to the 13 other care homes in the area as well as exploring with community nursing stakeholders and clinical commissioning groups how the tool could be used for older people receiving care in their own homes.

