Mrs Alice Evans is 58 years old. She is obese and has cardiometabolic syndrome, type two diabetes, elevated cholesterol and hypertension. Alice developed urinary incontinence and consulted a doctor. She was prescribed nitrofurantoin 100 mg twice daily for 3 days on the assumption that she had a urinary tract infection. Mrs Evans' medical records did not indicate that she had any symptoms of urinary tract infection and there was no record of a urine test. The incontinence persisted and Mrs Evans wanted to regain continence.
This article will explain how diabetes can affect bladder function, how to investigate the reasons why women develop urinary incontinence, and how the incontinence can be treated or managed.
Understanding normal bladder function
In order to void normally and to maintain bladder control, it is necessary to have a coordinated, sustained bladder contraction of adequate size and duration, a decrease in resistance of the bladder neck and urethra and no obstruction (Weledji et al, 2019). It is important to understand how the urinary tract normally functions in order to appreciate how diabetes affects these functions.
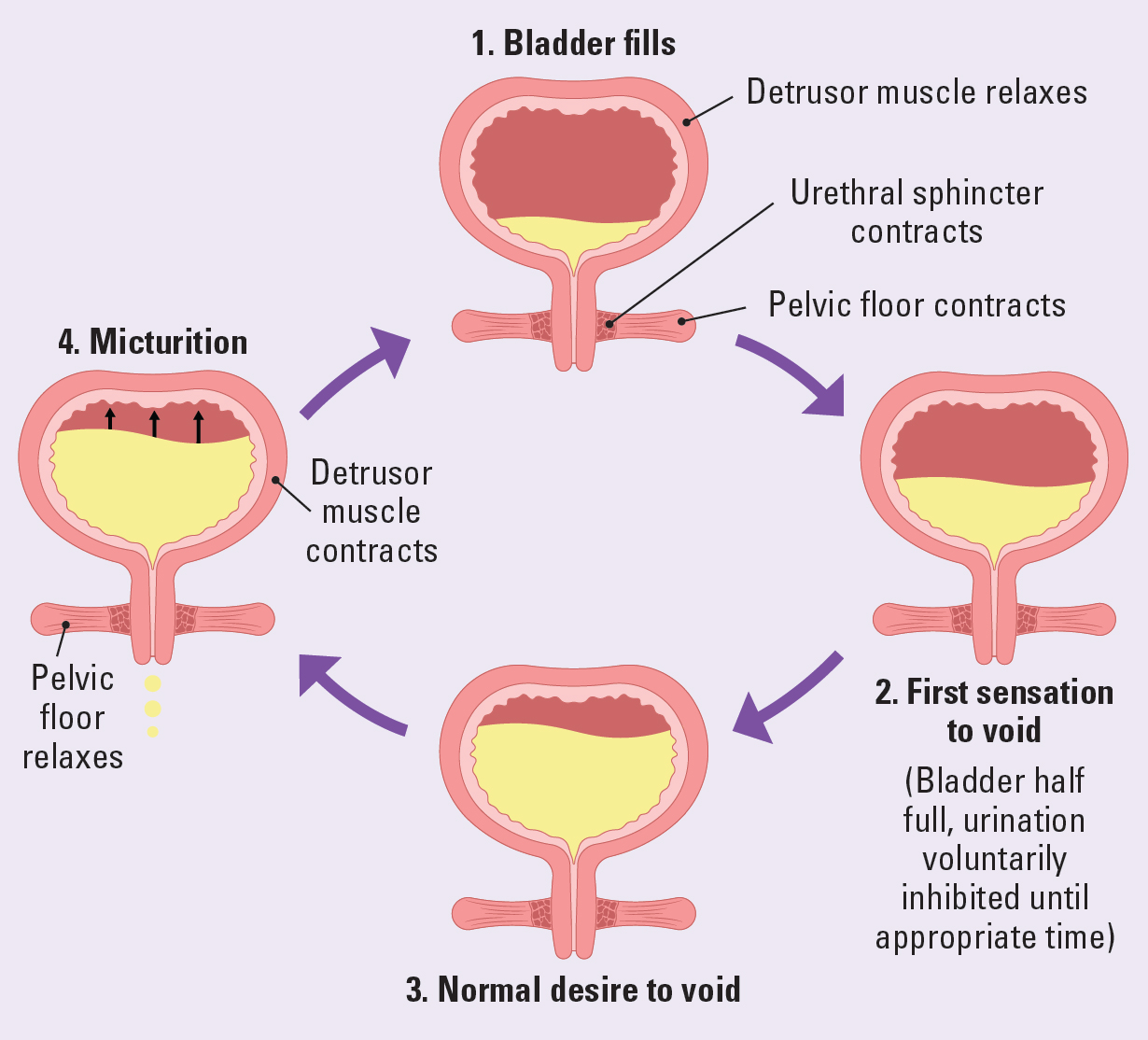
The bladder is a large hollow muscular organ that contains two muscles in the bladder: the detrusor and the trigone. The detrusor is the smooth muscle of the body of the bladder. The trigone is the triangular area between the ureteric orifices and the bladder neck. The detrusor stretches to allow the bladder to fill. It contracts to expel urine during bladder emptying (Fry and McCloskey, 2019). Figure 1 illustrates this.
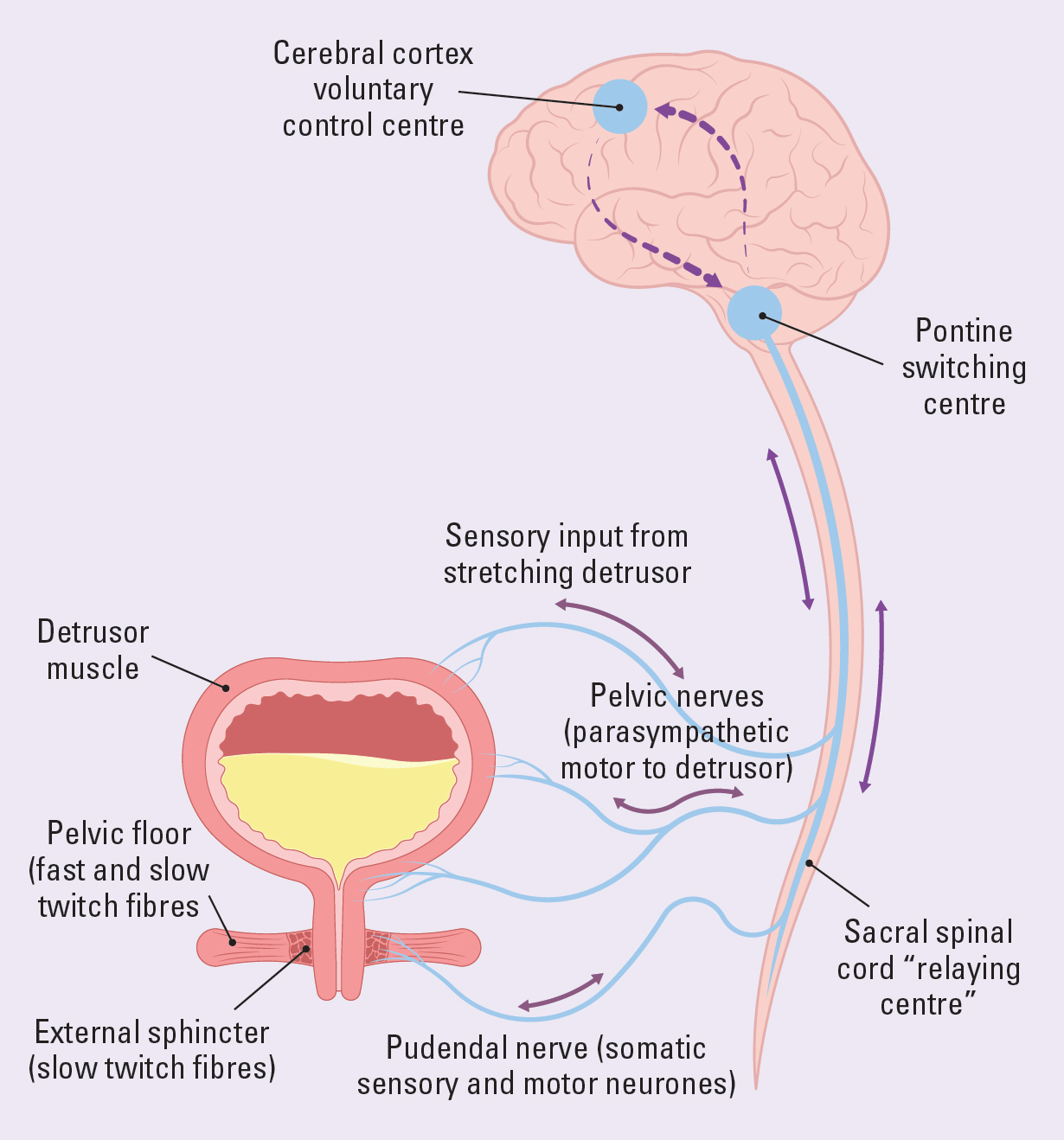
Bladder control is maintained by the sympathetic and parasympathetic systems. There are stretch receptors in the bladder wall that provide the brain with continuous feedback about the state of bladder fullness. The brain suppresses this information until the bladder is around 50% full. Adults are unaware of any sensation of bladder fullness until the bladder contains around 300ml of urine. Then, they can postpone the need to void until it is convenient. The micturition centre in the brain stem signals that the bladder is filling up. The micturition centre in the frontal lobe allows adults to inhibit urination. The bladder muscle relaxes and capacity is increased. The urethra remains tightly closed preventing leakage. When there is a need to urinate, the urethra relaxes and the bladder muscle contracts to expel urine. The autonomic nervous system and both micturition centres must function properly for adults to maintain continence (Fowler et al, 2008; Nazarko, 2010). Figure 2 illustrates normal bladder control.
How diabetes can affect bladder function
More than 4.3 million people in the UK have been diagnosed with diabetes and there are thought to be a further 850000 people living with diabetes who have not yet been diagnosed (Diabetes UK, 2024). Around half, over 2 million people, are at risk of diabetic neuropathy and bladder dysfunction (Blair et al, 2022). This nerve damage develops because of high blood glucose levels, while high levels of fats, such as triglycerides, damage the nerves and the blood vessels supplying the nerves (National Institute of Diabetes, Digestive and Kidney Diseases, 2024).
There are several types of neuropathy. The one that affects the urinary system is autonomic neuropathy. The autonomic nerves are part of the peripheral nervous system that regulates key functions within the body (such as the function of the heart, bladder, bowels), as well as bodily functions that are not consciously directed. The autonomic nervous system has two parts; the sympathetic nervous system that accelerates the heart rate, constricts blood vessels and raises blood pressure; the parasympathetic nervous system that slows the heart rate, increases intestinal and gland activity, and relaxes sphincter muscles. Urological complications of autonomic neuropathy include diabetic bladder dysfunction and recurrent urinary tract infections (Agochukwu-Mmonu et al, 2020). Autonomic neuropathy can affect the stretch receptors in the bladder and the sacral nerves that convey the sensation of bladder fullness to the brain (Vinik et al, 2003; Kumar and Biswas, 2022).
Bladder problems associated with diabetes are often referred to as diabetic cystopathy or diabetic bladder dysfunction (DBD). Prevalence varies and DBD is more common in people with poorly controlled diabetes and people who have had diabetes for a long time (Blair et al, 2022). Quality of life can be greatly impacted by DBD (Changxiao et al, 2014). Hypotonic bladder or underactive bladder and, less commonly, detrusor instability also known as overactive bladder can be caused by DBD.
It is thought that when a person first develops DBD the person develops overactive bladder, compensated bladder dysfunction. As diabetes progresses the person develops hypotonic or underactive bladder (Daneshgari et al, 2009; Yuan et al, 2015; Klee et al, 2019). DBD is a form of neurogenic bladder disease that can lead to urinary incontinence (de Groat and Yoshimura, 2015). Further research into how it can be prevented and treated is required (Yuan et al, 2015).
Assessment and diagnosis
Urinary incontinence is a symptom that, like any other, requires investigation and diagnosis in order to work out a treatment plan. The woman usually presents with a particular symptom or problem. A focused approach to assessment enables the nurse to gain further information and to begin to formulate a diagnosis. Assessment is restricted to specific body symptoms and aims to address presenting problems (Bickley and Szilagyi, 2012)
Normally assessment consists of baseline history, clinical examination, urine testing, bladder diary (also known as a frequency volume chart) and, in some cases, onward referral and a series of investigations including imaging, endoscopy and urodynamic investigations (International Continence Society, 2015; NICE, 2024a)
There are five components of assessment (detailed below and illustrated in Figure 3. These are:
- History taking to determine symptoms and identify any long-term conditions and how they impact the bladder
- Determining the type, frequency and severity of the problem by asking the patient to keep a bladder diary for 3 days. This records volume of fluid intake, type of fluid, urinary output, urinary frequency, degree of urgency and any urinary incontinence
- Assessment of functional and cognitive abilities if there are concerns that these are affecting continence
- Physical examination to identify any genito-urinary or general health problems impacting bladder function
- Medication review.
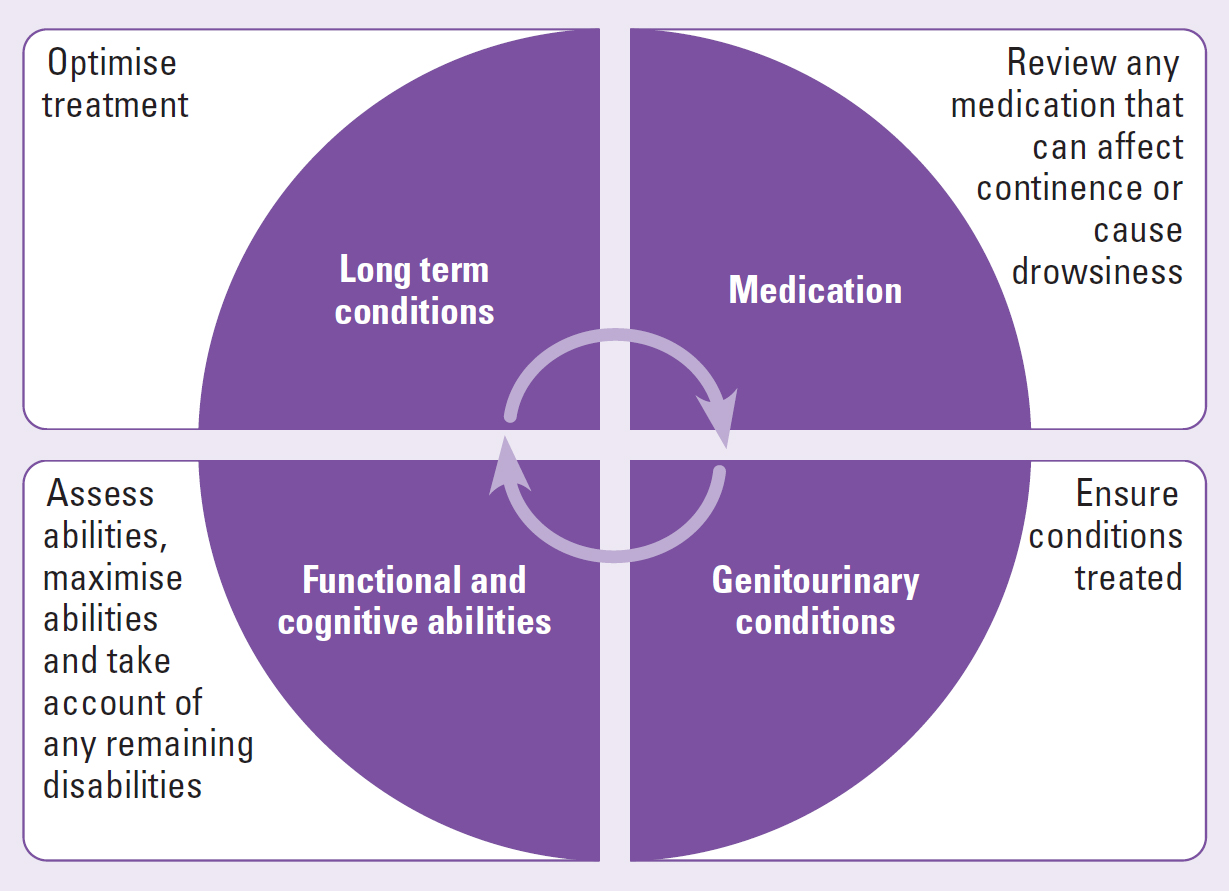
The components of assessment are determined by the level of assessment, the problems presenting and local policy. Core components of detailed assessments include history taking, the use of bladder diaries, usually for 3 days, and tests such as urinalysis and bladder scanning (NICE, 2024b).
The history and bladder diary often enable the nurse to determine diagnosis (Table 1).
Table 1. Common symptoms and possible diagnosis
| Type of symptom | Symptoms | Possible diagnosis |
|---|---|---|
| Storage, micturition and postmicturition | Dysuria, urinary frequency, suprapubic, tenderness, urgency polyuria haematuria | Infection, painful bladder syndrome |
| Storage | Urgency/frequency, nocturia, nocturnal polyuria, urge incontinence | Overactive bladder syndrome |
| Symptoms associated with sexual intercourse | Dyspareunia, vaginal dryness, incontinence during or just after intercourse | Oestrogen deficiency |
| Symptoms associated with genitourinary prolapse | Feeling of ‘something coming down’, low backache, heaviness, dragging sensation, stress incontinence | Genitourinary prolapse |
| Urinary incontinence |
|
|
| Voiding symptoms | Urinary retention, poor stream, hesitancy, intermittent stream, straining, terminal dribble | Detrusor dysfunction, outflow obstruction, dyssynergia |
| Postmicturition symptoms | Postmicturition dribble, feeling of incomplete emptying | Detrusor dysfunction, outflow obstruction, dyssynergia |
In Mrs Evans' case, she explained that her bladder had been ‘playing up’ for some years, and that she was ‘always going to the toilet’. She had had a few accidents but then things got much worse, and she lost all bladder sensation and control.
Physical examination
Physical examination should be carried out when clinically appropriate by a trained competent professional, in accordance with local policy. Ideally, this should include palpating the bladder after voiding to identify any urinary retention. In practice, this is easy on a slim woman but can be difficult in a woman who has a lot of abdominal fat. Residual urine that remains after voiding can be assessed using a bladder scanner. If one is not available, an intermittent catheter may be used. Bladder scanning is the preferred option because it is non-invasive. The nurse should examine the vagina in order to identify problems such as visible organ prolapse, atrophic vaginitis, pelvic floor weakness and any infections, such as candida infection.
Investigations include urinalysis, height, weight and body mass index (BMI), as well as checking alcohol consumption and whether the woman smokes cigarettes. A urinalysis enables the nurse to determine hydration levels by checking specific gravity as well as for possible infection and undiagnosed diabetes mellitus. The nurse should ask the patient about bowel habits and determine whether the woman suffers from constipation.
Mrs Evans had a BMI of 35, this is classed as obesity (NICE, 2023). Her urine showed glucose ++++. Blood pressure was 170/90. Blood tests revealed elevated cholesterol and a HbA1c of 105.
A HbA1c blood test is often used to diagnose or monitor type 2 diabetes. HbA1c measures glycated haemoglobin. When haemoglobin, the protein in red blood cells that transports oxygen, attaches to glucose in the blood the process is known as glycation. A HbA1c test measures the amount of glucose attached to the haemoglobin over a 2–3 month period, becasue this is how long the blood cells typically last for in the body (Medline plus, 2024). The World Health Organization (WHO) defines diabetes as having a HbA1c greater than 48 mmol/mol (WHO, 2020).
Testing for HbA1c provides an indication of average blood glucose levels over time. An elevated HbA1c level, indicates poor diabetes control and an increased risk of developing diabetes-related complications.
Mrs Evans' HbA1c indicated that her average blood glucose was around 16.2 mmol and that her diabetes was poorly controlled. A calculator to convert HbA1c to average blood glucose can be found at Diabetes.co.uk (https://www.diabetes.co.uk/hba1c-to-blood-sugar-level-converter.html). Mrs Evans had been prescribed 2 g metformin modified release once daily and gliclazide 80 mg morning and evening. She was asked whether she had been taking them. She replied that she had not taken them for some time and had been using ‘natural methods’ to control her diabetes.
A bladder scan showed a 550 ml of residual urine after voiding. Mrs Evans was wearing a small pad as she reported only passing small amounts of urine. She said that she did not mind how often she had to change the pad as long as she did not smell. She confessed that was ‘terrified of smelling of wee’.
Any medication that is affecting the ability to empty the bladder should be reviewed and discontinued if possible. Anticholinergic drugs such as oxybutynin and tolterodine may be inappropriately prescribed to a person because underactive bladder (UAB) may be misdiagnosed as overactive bladder (detrusor hyper-reflexia) resulting from symptoms of frequency and passing small amounts of urine (Nazarko, 2015). Researchers found that most people diagnosed with neurogenic bladder were taking anticholinergic medication: 63% were taking one medication and 9% more than one. A third of people in the study (n=15 415) with neurogenic bladder required hospital admission in a period of 1 year, over 21% were diagnosed with urinary tract infections, and around 8% were admitted with sepsis/septicaemia (Manack et al, 2011). Micturition is controlled by the central nervous system, which coordinates the sympathetic and parasympathetic nervous system activation with the somatic nervous system to the person maintain continence and pass urine normally. Any disturbance in coordination between CNS and the somatic nervous system results in a neurogenic bladder (Leslie et al, 2023). Underactive bladder is a type of neurogenic bladder dysfunction.
Mrs Evans was not taking her prescribed medication and had not taken her medication for some time. She stated that she was not taking any over-the-counter or herbal remedies.
Red flags and indications for specialist referral
It is important to balance clinical concerns against the risk of over-investigating women when there is no reason to suspect a serious underlying problem. Table 2 outlines red flags that indicate when specialist referral is required.
Table 2. Red flag signs and symptoms indicating urgent referral for investigation
| Visible haematuria |
| Microscopic haematuria (50 years or over) |
| Recurrent urinary tract infections (three or more infections in the past 6 months) |
| Loin pain |
| Suspected malignant mass |
| Recurrent catheter blockages (catheters blocking within 6 weeks of having been changed) |
| Hydronephrosis or kidney stones on imaging |
| Biochemical evidence of renal deterioration |
| Symptomatic prolapse at or below the introitus |
| Consider referral for: |
| Bladder/urethral pain |
| Benign pelvic mass |
| Faecal incontinence |
| Suspected neurological disease |
| Suspected fistulae |
| Previous continence surgery |
| Previous cancer surgery or radiotherapy |
Diagnosis and treatment
Mrs Evans has an underactive bladder (UAB). This is a prevalent but under-researched lower urinary tract symptom that typically occurs alongside detrusor under-activity (DU) (Wang et al, 2023). DU is defined as ‘a contraction of reduced strength and/or duration, resulting in prolonged bladder emptying and/or a failure to achieve complete bladder emptying within a normal time span’ (Abrams et al, 2003).
Knowledge of UAB is far from complete (Wang et al, 2023). It is unclear whether optimising diabetes control will improve bladder emptying. Treatment options are limited (Bayrak and Dmochowski, 2019). Treatment of any contributing factors, such as severe constipation or discontinuation of medication that has caused or contributed to DU can be helpful.
The person with UAB can try a number of techniques to encourage urination. Some people find warm flannels applied to the abdomen and gentle abdominal pressure helpful. Others find that applying suprapubic pressure, or scratching or stroking the thighs may be effective (Tidy, 2023).
Using a handheld vibrating device held over the bladder can stimulate contractions and avoid the need for catheterisation (Dasgupta et al, 1997; Prasad et al, 2003). Although there is little mention of these in the literature, they are reasonably priced at around £40 and the author has used them in practice for decades. In the author's experience, they can help 40–50% of people with voiding difficulties.
People who have hypotonic bladder often have reduced sensation and may be unaware of the need to urinate. In such cases, advising the person to try and urinate at specific intervals may help to reduce retention. Double voiding is a technique that aims to enable a person to fully empty the bladder. The person is advised to lean forward after voiding and try to urinate again. This is thought to facilitate bladder emptying (Miyazato et al, 2013). Figure 4 outlines treatment options in UAB.
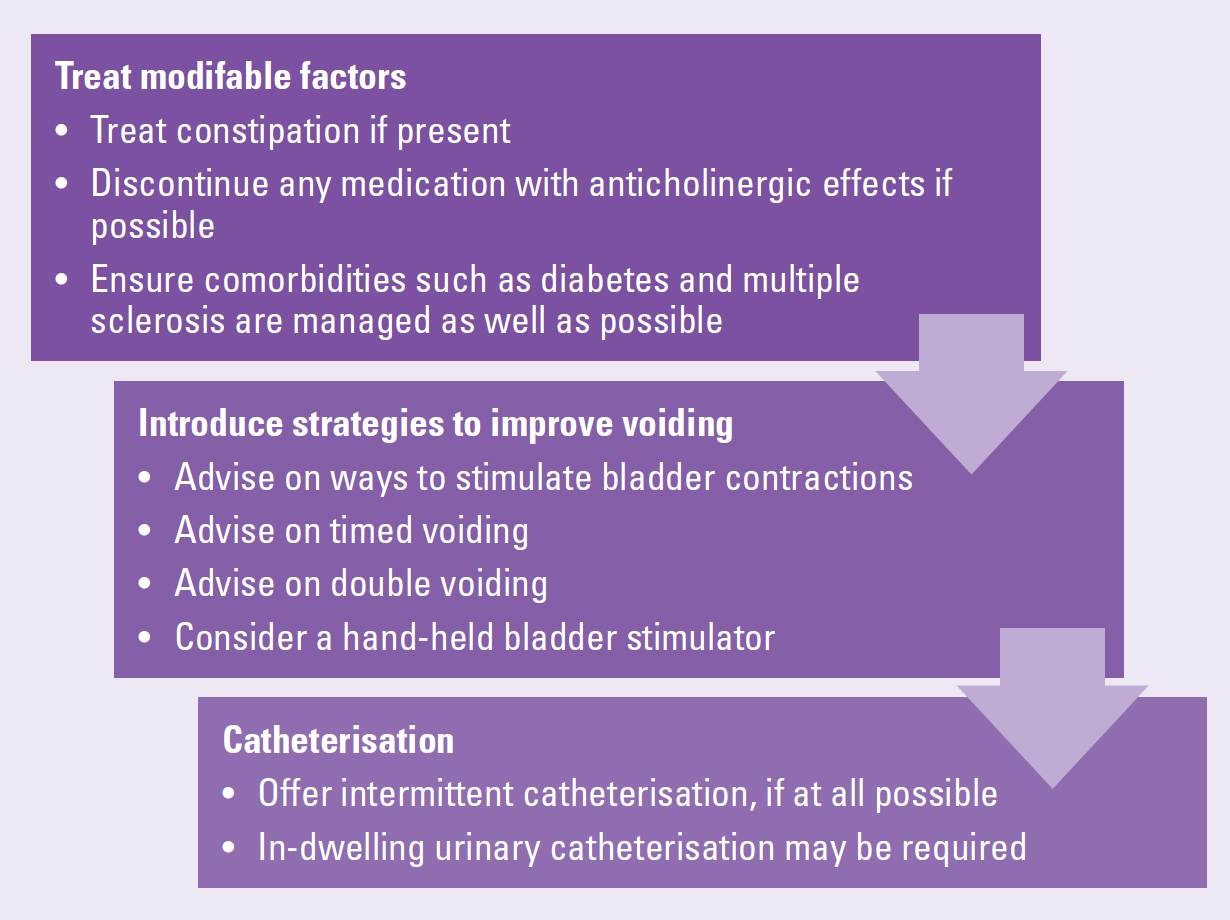
The preferred treatment for UAB is intermittent catheterisation (Arlandis et al, 2022). Sacral neuromodulation can be used as a third-line treatment in UAB (Feloney et al, 2024). Sacral neuromodulation (SNM) is a therapeutic technique that involves electrical stimulation to a sacral nerve root to modulate a neural pathway. It works like a pacemaker for the bowel or bladder. It is a minimally invasive procedure with good long-term outcomes and is used to treat bowel and/or bladder dysfunction. SNM involves assessment and, if it is suitable, implantation of a neurostimulator device. This is usually placed just beneath the skin in the upper buttock. The neurostimulator devices are about the same size as a £2 coin. A thin lead is also implanted in the lower back and connected to the device, along with the battery that lasts approximately 5 years (Goldman et al, 2018).
Discussion
It is not possible to determine the causes of urinary incontinence within a 10-minute GP consultation. Mrs Evans was inappropriately prescribed an antibiotic without clinical justification. It is vital that those of us entrusted to prescribe do so responsibly to reduce the growing threat of antimicrobial resistance (UK Government, 2024) and to reduced the issues associated with antibiotic prescribing, such as allergies and gastrointestinal side effects.
As the number of people with diabetes grows, the number of people with DBD is set to rise. It will be necessary to ensure the availability of services to diagnose and treat DBD.
Outcome
Recent research has led to NHS England introducing a new programme to enable the remission of type 2 diabetes due to weight loss, the NHS Type 2 Diabetes Path to Remission Programme (NHS England, 2024). Mrs Evans would be able to join this programme and, if sufficient weight was lost, may no longer require medication for her diabetes. Mrs Evans was keen to try this and agreed to start taking her diabetes medication and medication targetting blood pressure. She was not willing to take her statin and said she feels ‘much better without it’.
She has agreed to intermittent catheterisation and quickly mastered the technique. She said:
‘It has given me my life back. All I've worried about for ages was wetting myself in public or smelling.’
Effectively assessing women with diabetes reporting incontinence, and diagnosing and treating DAB, can alleviate women's symptoms and improve their quality of life.
Key points
- Underactive bladder is an under-recognised cause of urinary incontinence
- The number of people with underactive bladder is set to rise in line with the increase in people with diabetes
- The NHS must ensure that services are available to diagnose and treat underactive bladder
- Treatment options are limited and further research is required
- Underactive bladder can have a devastating effect on a person's life
CPD reflective questions
- UAB develops because of poorly controlled diabetes. How can you help your patients who have diabetes to manage diabetes well?
- Bladder dysfunction is common in people with diabetes. Do you think that we should screen for urinary incontinence as part of diabetes reviews
- What skills and resources do you require to enable you to assess the person with diabetes and bladder problems?


