Dementia is a syndrome, a term that is used to describe a group of symptoms. These symptoms affect a person's ability to interpret and perceive the world and to communicate with others. The World Health Organization's (WHO) definition of dementia is:
Dementia is a syndrome—usually of a chronic or progressive nature—in which there is deterioration in cognitive function (ie the ability to process thought) beyond what might be expected from normal ageing. It affects memory, thinking, orientation, comprehension, calculation, learning capacity, language and judgement. Consciousness is not affected. The impairment in cognitive function is commonly accompanied, and occasionally preceded, by deterioration in emotional control, social behaviour or motivation.
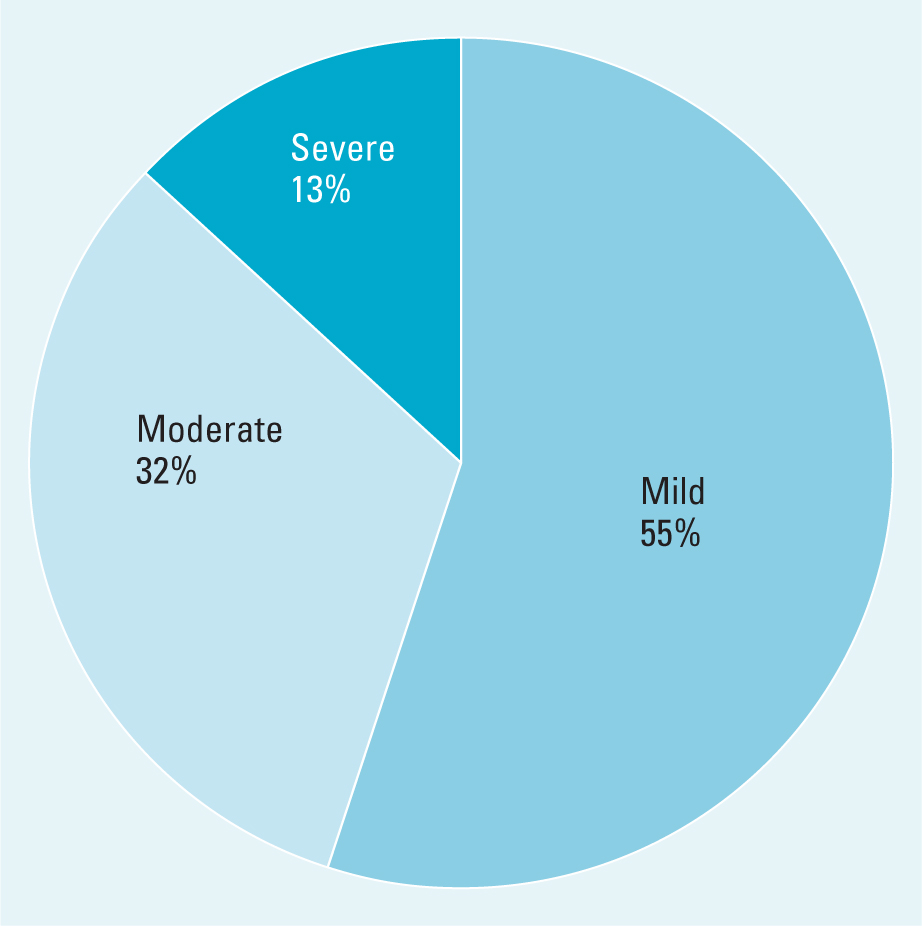
In the UK, more than 9 82 000 people are living with dementia (Alzheimer's Society, 2024a). Most people living with this illness are aged 65 years and over and have late onset dementia. Research indicates that over half of these patients have mild dementia, around a third have moderate dementia and an eighth have severe dementia (Prince et al, 2014; Wittenberg et al, 2019) (Figure 1).
Most people who develop dementia are older and are likely to develop other age-related changes that may, if left untreated, affect the ability to function to capacity. People with dementia may struggle to make sense of the world, manage their health and communicate. Age-related changes can affect the ability to see, hear and move around freely (Alattar et al, 2020; Freiberger et al, 2020).
Certain long-term conditions such as diabetes, heart failure and hypertension become more prevalent as a person ages (National Institute for Health and Care Excellence, 2018; 2020; Public Health England, 2017a; 2017b). If these long-term conditions are not managed well, they can impact on general health and worsen the effects of dementia.
Ageing also influences the immune system and as people age, they are at a greater risk of developing infections. This article examines ways to minimise the effects of age-related changes and long-term conditions, and to enable the person with dementia to enjoy the best possible quality of life.
Effects of ageing on hearing
There are over 18 million adults in the UK who are deaf, have tinnitus or hearing loss (Royal National Institute for Deaf People, 2024). Hearing loss becomes more common as people age and 80% of all people aged 70 years and over may have some hearing loss (Akeroyd and Munro, 2024; Royal National Institute for Deaf People, 2024). Hearing loss usually develops slowly and the person may initially be unaware of his or her hearing loss. The person may struggle to take part in conversations and can easily become isolated, lonely and depressed.
There are three components to managing hearing loss:
When hearing loss is suspected, the person's GP may check the ears for wax and refer for a hearing test, if necessary. If wax is causing hearing problems, it can be removed. The person's hearing can be tested and hearing aids issued if needed. The person may need encouragement to use hearing aids and, in some cases, may need help to put them in. Care givers and health professionals can use a range of strategies including cutting background noise to compensate for remaining disability (Further information available in Resources).
Effects of ageing on vision
Ageing leads to visual changes and an increase in eye diseases. The first age-related change to affect adults is presbyopia. In young people, the lens in the eye is flexible and enables people with normal vision to see near and far objects. As the lens ages it becomes less flexible and most adults struggle to see things that are near them. Presbyopia develops from the age of 40 years and stabilises at the age of 65 years. Presbyopia can be treated with reading glasses, contact lenses, laser surgery or intra-ocular lens replacement (NHS England, 2023).
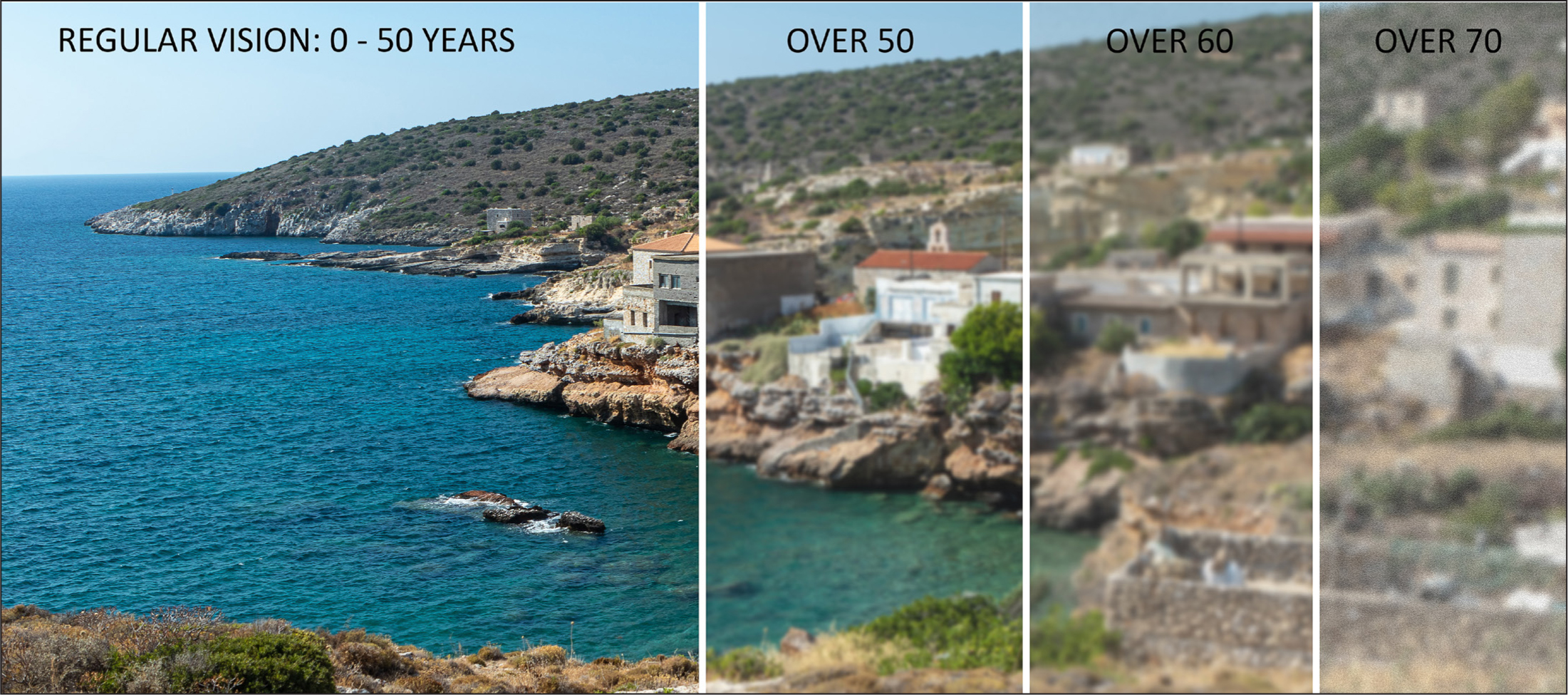
Ageing affects the ability to see in low light as the ciliary muscle that enables the pupil to dilate in response to low light and to contract in response to bright light becomes atrophied and less light reaches the eye. The lens of the eye, which is crystal clear in youth, becomes yellow (Pescosolido et al, 2016). These changes make it difficult for an older person to move from a brightly-lit area to a darker one (Rukmini et al, 2017). Yellowing of the lens leads to increased difficulty in seeing colours and contrasts. Figure 2 shows an image as seen through the eyes of people aged below 50 years, over 50 years, over 60 years and over 75 years. This clearly illustrates the loss of contrast and brightness caused by the ageing lens of the eye.
There are four components to managing visual changes:
More than 6 million people in the UK are living with uncorrected refractive error and sight threatening conditions, and many are unaware of any visual impairment (Royal National Institute for Blind People, 2024). More than two million people have sight loss that has a significant impact on their daily lives (Royal National Institute for Blind People, 2024).
Eye tests are crucially important. Older people should have eye tests at least every two years and some people may require more frequent testing. If an individual is unable to attend the opticians because of illness or disability, the eye test can be carried out at home. Many of the common causes of vision loss in older people, such as cataracts and glaucoma, are treatable especially when diagnosed early (Bonnielin et al, 2020). Many visual problems can be treated with up-to-date spectacles that enable a person to see as well as possible.
Changes to the environment can compensate for other alterations. An older person needs brighter light to see clearly. Using diffused lighting, task lighting and fixtures that minimise glare may enable the person to see well (Akpek and Smith, 2013).
Changes to the lens of the eye make it difficult to distinguish objects from their background. The use of contrast can enable the person to retain their vision. Simple changes such as using dark towels in a light bathroom and a dark toilet seat on a white toilet can help. In the kitchen, using a white chopping board for dark foods and a dark board for light foods may encourage independence and increase safety. Painting the architrave of the door in a contrasting colour may help the person to see better. Brightly coloured tape can be used to highlight steps. If rugs are used, ensure contrast between the floor and the rug and use non-slip backings.
Vision and hearing wellbeing and reduced risk of dementia
Evidence suggests that uncorrected visual impairment is associated with an increased risk of developing dementia. One study found that visual impairment was associated with 2–5 times increased risk of developing dementia (Tran et al, 2020). More severe visual impairment was associated with increasingly elevated risk of incident dementia. The researchers commented that visual impairment may be a risk factor in dementia but recommend further research with a larger sample of people. They also called for research to evaluate the effect of specific ophthalmic interventions on people with dementia (Tran et al, 2020).
Matthews et al (2024) found that people with poor vision and hearing socialised less often, were less mobile and more likely to be depressed. They commented that actions to promote a healthy lifestyle, reduce depression and foster social engagement of older people with sensory impairments were likely to be beneficial in preventing cognitive decline and dementia. Correcting visual loss reduces the risk of dementia (Alzheimer's Society, 2024b). There can be an overlap in symptoms of dementia and cataract (Jefferis et al, 2011). In some cases, people who have dementia and cataracts improve following cataract surgery (Gray et al, 2006). Case history 1 illustrates this aspect.
Case history 1
Mrs. Ethel Harris, who had dementia, was admitted to the hospital after sustaining a fractured wrist in a fall. Mrs Harris' wrist was badly swollen, so she was admitted to the hospital until the swelling reduced enough for her to receive a full cast. Mrs Harris was extremely confused, wandered into other people's rooms and tried to get into bed with other patients. She was clearly hallucinating and had conversations with people who were not there. The day after her admission to the hospital, her daughter informed the staff that her mother was supposed to attend the eye unit for cataract surgery. The staff on the ward wondered whether surgery would be beneficial, considering the severity of Mrs Harris' dementia.
Following the surgery, Mrs Harris was very quiet and remained in bed. The next morning she appeared more orientated and less distressed. In the evening, the nurse helped her change into her night clothes after which she sat quietly and watched television. She told the staff, ‘I have been so cut off. I couldn't see, my hearing is not good and I'm losing my memory. At least now I have some chance of working out what's going on’.
Note: Patient's name and details have been changed to protect patient confidentiality.
Ageing's effects on mobility
Ageing is associated with reduced muscle function and strength and a reduction in aerobic capacity—a measure of the ability of the heart and lungs to supply oxygen to the muscles (Wilkinson et al, 2018). Being active maintains bone and heart health as good circulation enables the person to maintain their ability to dress, clean, cook and perform other daily activities. Physical activity also reduces the risk of falls by improving balance and strength.
Exercise and physical activity can enable the person to meet other people, retain connections with friends and can reduce the risks of isolation and depression. Exercise also helps a person sleep better and improves the overall quality of sleep (Alzheimer's Society, 2024c).
Long-term conditions
People with dementia often have other long-term conditions. Type 2 diabetes is associated with an increased risk for cognitive decline, mild cognitive impairment, vascular dementia and Alzheimer's type dementia (Morgan et al, 2024). Hypoglycaemic episodes deprive the brain of glucose and contribute to cognitive decline. Poor blood glucose control also increases glycation, the process of glucose and protein binding together. Glycation leads to thickening in the blood vessels and a reduction on blood flow. These changes cause damage to the small blood vessels in the brain and reduced blood flow. Damage to the large vessels of the brain can be caused by glycation, hypertension and elevated levels of cholesterol. These changes are believed to further increase cognitive decline (Nguyen et al, 2014: Simó et al, 2017). Cognitive decline then impairs a person's ability to manage diabetes, leading to poorer glycaemic control, increased risk of hypoglycaemia, further decline and poorer prognosis (Bordier et al, 2014).
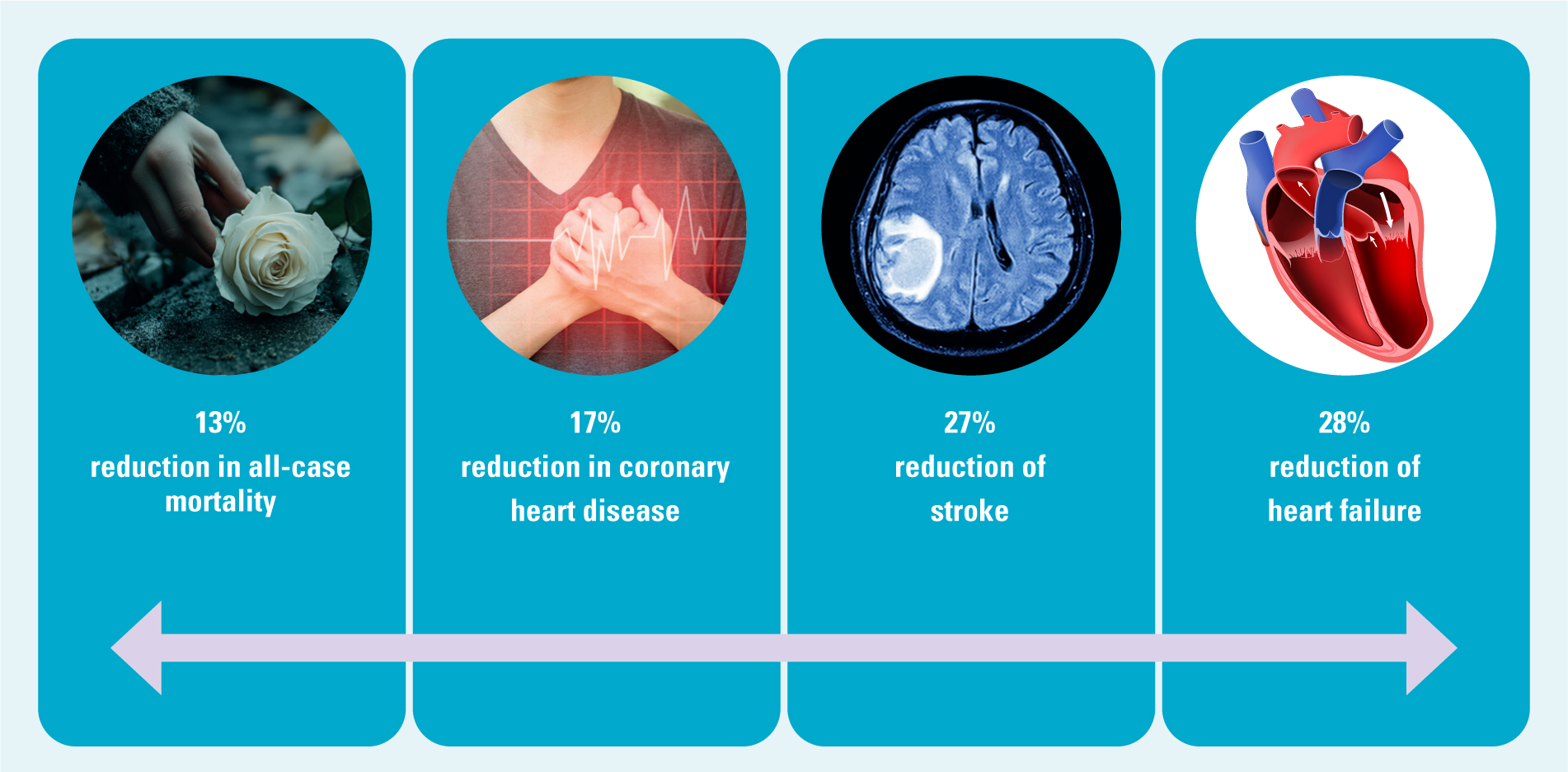
Hypertension becomes more common as people age; 60% of older adults have hypertension and it is twice as common in people with diabetes (NHS Digital, 2023). A 10 mmHg reduction in blood pressure lowers all-cause mortality by 13%, coronary heart disease by 17%, stroke by 27% and heart failure by 28% (Agyemang et al, 2015) (Figure 3). Supporting and enabling a person with dementia to manage long-term conditions such as diabetes can slow the rate of cognitive decline and enable the person to enjoy the best possible health.
The ageing immune system
The immune system becomes less effective as people age and this vulnerability increases the risk of infection (Tran et al, 2023). People with dementia are especially vulnerable to infections, and pneumonia is a common cause of death among them (Yao et al, 2024). Encouraging and enabling the person with dementia to have relevant vaccinations such as the pneumonia, flu and covid, shingles and respiratory syncytial virus vaccines may protect the them from infection and improve their quality of life. The resources section provides details of the Green Book on immunisations.
Maintaining a sense of self and hopefulness
A diagnosis of dementia can seem like a death sentence. The person's hopes and dreams can come crashing down, plans to travel or to enjoy certain activities in retirement can turn to dust. The reality is that people with Alzheimer's disease may live for 8-10 years, while people with vascular dementia may live for around 5 years (Alzheimer's Society, 2024d). The community nurse can use hope-based interventions to help the person with dementia, and family can help in refocusing goals and finding joy in certain aspects of life (Pepper et al, 2024). The person who enjoys running and has been diagnosed with dementia may still be able to run with support. Retaining the ability to carry out an enjoyable activity has positive effects on the person's physical and mental health.
Discussion
People who have dementia may have mild, moderate or severe symptoms. Each person with dementia is affected differently; however, all experience difficulty in planning, communicating and making sense of the world in general. Dementia rarely occurs in isolation. The person with dementia experiences age-related changes that affect vision and hearing. The individual will usually have a number of long-term conditions. The person may require simple interventions to enable them to function at a higher level and to experience the best possible quality of life.
A range of services from different professionals may be required. A pharmacist's advice may be required to minimise medication, simplify medication regimes and organise monitored dosage if required. An occupational therapist may assess difficulties in managing daily activities, provide equipment to support independence and offer guidance on care needs. A social worker may assess and organise supportive care and a dietician's advice may also be necessary. The community nurse can assist the person living with dementia on an individual level, while liaising with the patient's family, caregivers and specialists. The professional overview of a person's complex health and social care needs is invaluable and can make a real difference to the care of the individual.
Conclusions
It is important that community nurses are aware of age-related changes and how they impact a person living with dementia. Working with the older person, family and caregivers can ensure that the person receives individualised care to enjoy the best possible quality of life. The early implementation of these measures can go a long way.


