Hypertension and type-2 diabetes mellitus (T2DM) are two of the most common long-term conditions worldwide. Hypertension, as one of the main causes of chronic cardiovascular conditions, caused 9.4 million deaths and 7% of the morbidity burden expressed in disability-adjusted life-years in 2010. Similarly, it has been estimated that approximately 4.2 million people died from T2DM in 2019 (International Diabetes Federation (IDF), 2019). Both pathologies lead to severe complications, disabilities, death and high healthcare costs (Buffel du Vaure et al, 2016).
Despite important advances in the treatment of chronic diseases like hypertension and T2DM, lack of adherence to therapeutic regimens by patients remains a challenge for health systems, and it has been often cited as a barrier to controlling cardiovascular diseases (Ministério da Saúde do Brasil, 2016). Various studies have reported medication adherence rates of 52%–74% in those with hypertension and 36%–93% in those with T2DM (Chang et al, 2015). Additionally, from non-pharmacological aspects, adherence to physical activity has been reported to be between 33.2% and 25% in patients with diabetes (Mumu et al, 2014; Saleh et al, 2014) and 68.8% in those with hypertension (Tibebu et al, 2017). Similarly, adherence to diet has been reported to be between 44.8%–88% in those with diabetes (Mumu et al, 2014; Saleh et al, 2014) and 30.9% in those with hypertension (Tibebu et al, 2017). Consequently, clinical results can be unfavourable, such as re-hospitalisation, exacerbation of other chronic diseases and higher medical care costs (Verloo et al, 2017). In addition, lack of adherence to lifestyle modifications among patients with diabetes leads to short-term risks and long-term complications, as well as decreasing quality of life (Saleh et al, 2014).
In this context, different ways of measuring adherence to therapeutic regimen have been proposed, but most studies have focused on pharmacological aspects, excluding the integral aspects for adequate control of chronic diseases, such as recommendations related to diet, physical activity and control of other risk factors (smoking, obesity, etc.) (López et al, 2016).
Many interventions intended to improve adherence to therapeutic regimen have been found to have positive effects in controlling hypertension and T2DM. Among these, educational interventions using various strategies with multifaceted approach have been emphasised, and these have been found to be most effective (Conn et al, 2015; Sapkota et al, 2015). The teach-back method has demonstrated effectiveness in a broad spectrum of medical outcomes, evidencing better outcomes in disease-specific knowledge, adherence and self-efficacy (Ha Dinh et al, 2016). Similarly, nurse-led interventions and collaborative interventions between nurses and other members of health staff have shown to moderately improve adherence in older adults (Verloo et al, 2017).
With this in mind, and aiming to support the nurse's role in cardiovascular risk programmes and implement the most effective interventions in this area, a multifaceted intervention involving the ‘teaching:individual’ nursing intervention classification label was designed by using different strategies to improve adherence to both pharmacological and non-pharmacological therapeutic regimens. The specific aims of the study were: (1) to evaluate the efficacy of the individual teaching nursing intervention (Bulechek et al, 2012) compared with usual care (control group), in order to improve adherence to the therapeutic regimen in people with hypertension, T2DM or both; and (2) to analyse the impact of nursing interventions to decrease systolic blood pressure (SBP) and glycated haemoglobin (HbA1c) levels in people with hypertension and T2DM.
Methods
This study was a single-blind, randomised clinical trial with a two-arm, parallel-group design. Participants were medically diagnosed with hypertension and type 2 diabetes mellitus, were recruited from programs for the control of cardiovascular risk factors on primary care. The trial protocol was registered at ClinicalTrials.gov under registration number NCT02758275, and all the methodological aspects related to this study have been previously published (Romero et al, 2019).
Intervention
The intervention was multifaceted, with educational, behavioural and affective components (Sapkota et al, 2015). The educational component consisted of the transmission of information about the disease process, treatment and control of risk factors, among others, using the intervention ‘teaching: individual’, as strategies, written material and devices for ordering medications and schedules. The behavioural component focused on changing unhealthy habits or reinforcing positive behaviours. In the affective component, participants were encouraged to express feelings related to the experience of living with the disease and its treatment. The nurses taught about behaviour modification, disease process and prescription medications, prescribed diet, prescribed exercise, and coping enhancement (Romero et al, 2019).
Statistical analysis
Analyses were based on intention to treat. Summary statistics comparing randomised arms at baseline were tabulated: categorical and continuous variables were compared using chi-squared or Fisher exact tests and Student's t-test or Mann-Whitney U-test, respectively.
To use repeatedly measured data and investigate changes in an outcome over time and compare these changes among treatment groups, a linear marginal model with an exchangeable correlation matrix was used for repeated measures of SBP and generalised estimating equations (GEE) was used for repeated measures with an unstructured correlation matrix (treatment adherence and HbA1c levels), using all available data (Albert, 1999; Ma et al, 2012). Models predicting outcomes from treatment group, time and the treatment group by time interaction were used. All analyses were conducted using STATA software version 15.0; p-values <0.05 were considered statistically significant.
Sensitivity analyses were conducted. It is known from studies that blood pressure measured at home or that measured without the presence of medical assistants is 10–15 mmHg lower than laboratory-measured blood pressure (Myers et al, 2012). Therefore, SBP was measured as automated office blood pressure, using a WatchBP 03-microlife device in the casual mode. Similarly, a sub-analysis was performed on SBP for 24 hours in participants with more than 70% correct measurements by ambulatory blood pressure monitoring, as recommended by the hypertension guidelines (Williams et al, 2018).
Results
A total of 200 patients were randomised, with 98 assigned to the individual teaching group and 102 to the usual care group. Some 23 patients refused to participate, the main reason being their refusal to use the ambulatory blood pressure monitoring device. Sociodemographic and clinical characteristics were similar between those who agreed and those who did not agree to participate in the study, except for age. Some 186 participants (93.0%) completed the 12-month follow-up visit and were included in the analysis; however, the adherence score was measured in 96.5% of the participants, the 24-hour SBP, in 84.8% and the HbA1c, in 96.2% (Figure 1).
 Figure 1. CONSORT flowchart showing the flow of participants throughout the trial.
Figure 1. CONSORT flowchart showing the flow of participants throughout the trial.
There were no significant differences in sociodemographic and clinical characteristics between the intervention and control groups; these results have been published previously (Romero et al, 2019).
The mean (SD) age of the individual teaching group was 62.8±11.1 years, and most were women 73.0% (n=146); 62.5% (n=125) were diagnosed with hypertension, 12.0% (n=24) had T2DM and 25.5% (n=51) had both. These participants had a mean (SD) adherence score of 9.39±2.05 points, their SBP in 24 h was 124±14.3 mmHg, HbA1c levels were 6.18±1.58%, SBP (automated office blood pressure) was 136±19.5 mmHg, and SBP in 24 h (70% correct measurements) was 124±14.0 mmHg.
The mean (SE) adherence score at 6 months was 10.73 (0.20) points in the individual teaching group and 9.86 (0.20) in the usual care group, and, at 12 months, it was 10.43 (0.21) and 10.03 (0.20) points, respectively (Figure 2A). The difference in mean adherence score change at 6 months was greater in the individual teaching group compared with the usual care group (mean difference=0.87 points; 95% CI, 0.30–1.44; p= 0.003). In addition, the adherence score at 12 months was higher in the individual teaching group compared with the usual care group; however, this difference was not statistically significant (mean difference=0.39 points; 95% CI, -0.21 to 0.99; p=0.199) (Table 1).
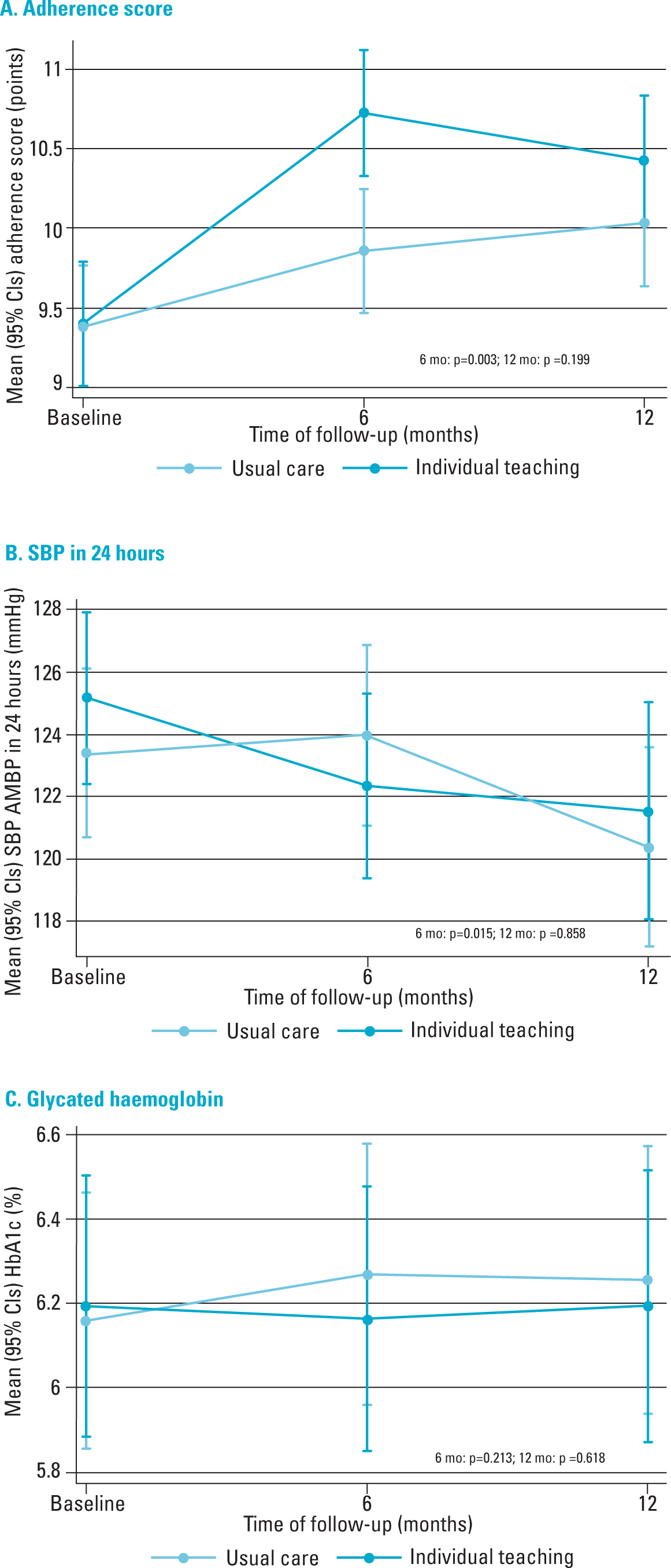 Figure 2. Change in mean adherence scare, SBP and HbA1c for the individual teaching and usual care groups
Figure 2. Change in mean adherence scare, SBP and HbA1c for the individual teaching and usual care groups
Table 1. Effect of the intervention on adherence, SBP and HbA1c in individuals with hypertension and/or T2DM
| Individual teaching group | Usual care group | Treatment comparison | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 6 months | 12 months | |||||||||
| Outcomes | Baseline | 6 months | 12 months | Baseline | 6 months | 12 months | Difference 95% CI | p | Difference 95% CI | p |
| Adherence score (points) | 9.40 (0.20) | 10.73 (0.20) | 10.43 (0.21) | 9.38 (0.19) | 9.86 (0.20) | 10.03 (0.20) | 0.87 (0.30 to 1.44)b | 0.003 | 0.39 (-0.21 to 0.99)b | 0.199 |
| SBP in 24 hours (mmHg) ABPM | 125 (1.41) | 122 (1.51) | 121 (1.77) | 123 (1.38) | 124 (1.48) | 120 (1.63) | -3.79 (-6.85 to -0.73)c | 0.015 | -0.31 (-3.69 to 3.08)c | 0.858 |
| HbA1c (%) | 6.19 (0.16) | 6.16 (0.16) | 6.19 (0.16) | 6.16 (0.15) | 6.27 (0.16) | 6.26 (0.16) | -0.16 (-0.41 to 0.09)b | 0.213 | -0.06 (-0.32 to 0.19)b | 0.618 |
| Sensitivity analysis | ||||||||||
| SBP AOBP (mmHg)d | 136 (2.07) | 128 (2.23) | 130 (2.62) | 135 (2.05) | 135 (2.16) | 134 (2.38) | -7.49 (-13.76 to -1.22)c | 0.019 | -3.27 (-10.18 to 3.65)c | 0.353 |
| SBP in 24 hours (mmHg) ABPMe | 125 (1.41) | 122 (1.55) | 122 (1.80) | 123 (1.39) | 124 (1.50) | 121 (1.67) | -4.58 (-7.79 to -1.37)c | 0.005 | -0.90 (-4.43 to 2.63)c | 0.616 |
Means and standard errors reported at baseline, 6 months and 12 months
bAnalysis generalized estimating equations (GEE) for repeated measures with an unstructured correlation matrix
cAnalysis linear marginal model with an exchangeable correlation matrix for repeated measures
dSystolic blood pressure (SBP) measured as automated office blood pressure (AOBP)
eSystolic blood pressure in 24 h in participants with more than 70% correct measurements in ambulatory blood pressure monitoring (ABPM)
The mean (SE) SBP in 24 hours by ambulatory blood pressure monitoring change at 6 months was 122 (1.51) mmHg in the individual teaching group and 124 (1.48) mmHg in the usual care group, and, at 12 months, it was 121 (1.77) vs. 120 (1.63) (Figure 2B). The mean difference in SBP in 24 hours at 6 months between the individual teaching and usual care groups was -3.79 mmHg (95% CI, -6.85 to -0.73, p = 0.015), indicating a significant reduction in SBP in the intervention group, but the effect at 12 months was not significant (mean difference = -0.31 mmHg; 95% CI, -3.69 to 3.08; p = 0.858) (Table 1). The mean differences in HbA1c at 6 and 12 months of follow-up between the individual teaching and usual care groups were not significant (-0.16% 95% CI, -0.41 to 0.09; p = 0.213 and -0.06% 95% CI, -0.32 to 0.19; p=0.618, respectively) (Figure 2C and Table 1).
The mean (SE) SBP automated office blood pressure change at 6 months was 128 (2.23) mmHg in the individual teaching group and 135 (2.16) mmHg in the usual care group, and, at 12 months, it was 130 (2.62) and 134 (2.38) mmHg, respectively (Figure 3A). The difference in mean SBP measured by automated office blood pressure at 6 months of follow-up between the individual teaching and usual care groups was -7.49 mmHg (95% CI, -13.76 to -1.22; p=0.019), achieving a significant reduction in SBP figures in the intervention group. At 12 months, the difference in mean SBP was -3.27 mmHg (95% CI, -10.18 to 3.65; p=0.353); however, this difference was not statistically significant (Table 1).
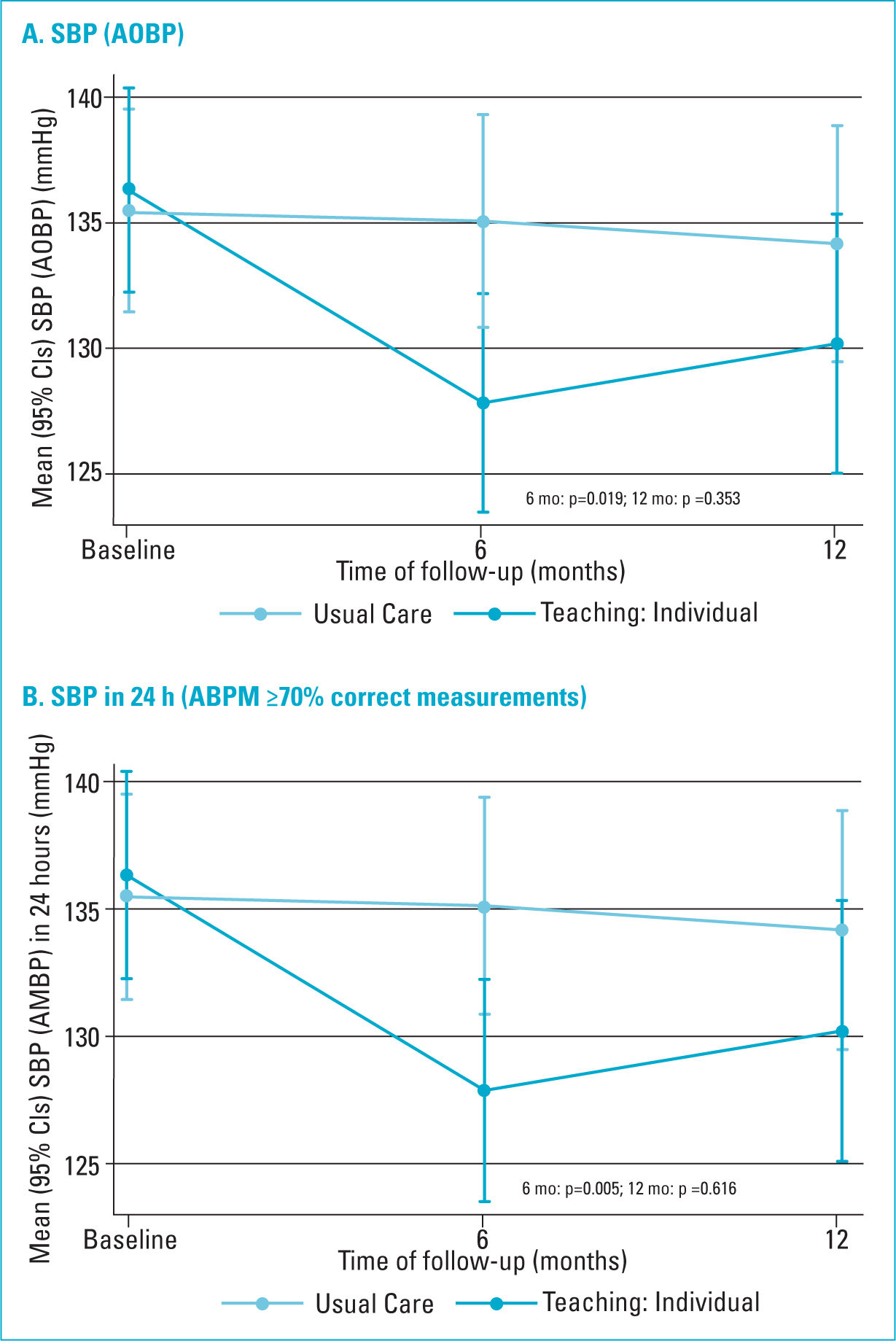 Figure 3. Change in mean SBP (AOBP and ABPM) for the Teaching: Individual and Usual Care groups.
Figure 3. Change in mean SBP (AOBP and ABPM) for the Teaching: Individual and Usual Care groups.
The mean (SE) SBP in 24 hours ambulatory blood pressure monitoring in participants with more than 70% correct measurements at 6 months was 122 (1.55) mmHg in the individual teaching group and 124 (1.50) in the usual care group, and, at 12 months, it was 122 (1.80) mmHg in the individual teaching group vs. 121 (1.67) mmHg in the usual care group (Figure 3B). The difference in mean SBP change in 24 hours decreased in the individual teaching group compared with the usual care group at 6 months (mean difference=-4.58 mmHg; 95% CI, -7.79 to -1.37; p=0.005), and at 12 months (mean difference=-0.90 mmHg; 95% CI, -4.43 to 2.63; p=0.616) (Table 1).
Discussion
Although, at the beginning of the study, the participants' variables were within normal parameters, the results proved that the individual teaching nursing intervention improved adherence to treatment and yielded a significant reduction in SBP in 24 hours, with both ambulatory blood pressure monitoring and automated office blood pressure at the 6-month follow-up; however, the reduction was not significant at 12 months, nor was it significant for HbA1c levels at any of the follow-up times.
The intervention in this study was a multifaceted one, involving different adherence aspects; additionally, it was conducted only by nursing professionals through individual face-to-face sessions with each of the participants in the intervention group. Considering these aspects on the outcomes of interest, the results are consistent with findings from other recent studies. For example, a systematic review of interventions on adherence to anti-diabetic medications in patients with T2DM determined that multifaceted interventions, involving various factors of non-adherence to medication, were more effective in improving adherence with the pharmaceutical regimen and achieve glycaemic targets compared with single-component strategies (Sapkota et al, 2015).
Similarly, a systematic review that evaluated the effect of nursing interventions to improve adherence to medication for older adults living at home and who were discharged established that interventions guided by nurses and in collaboration with nursing staff moderately improved adherence among the subjects (Verloo et al, 2017). Another systematic review supported the teach-back method to maximise comprehension of the disease, promote knowledge, adherence, self-efficacy and self-care skills on educating people with chronic diseases (Ha Dinh et al, 2016).
Regarding the effect on blood pressure, this study found similar results to those reported in a systematic review that showed that interventions aimed at patients, with multiple and motivational educational sessions to modify lifestyles and adhere to medication, yielded a mean change in SBP of -3.9 mmHg (95% CI, -5.4 to -2.3) (Mills et al, 2018). In addition, it has been shown that interventions designed to decrease blood pressure that support usual medical care, where only nurses or non-medical staff are involved, are effective in achieve control of blood pressure. However, it is important to highlight that these interventions were more effective when they were multidisciplinary (Clark et al, 2010; Mills et al, 2018).
In relation to the effect of educational interventions on decreasing glycated HbA1c levels, the results are divergent. In contrast to the present study's results, a review of 120 publications of 118 unique interventions found 61.9% (73/118 interventions) significant changes in HbA1c with average absolute reduction of 0.57% (Chrvala et al, 2016). Similarly, a meta-analysis of 13 randomised clinical trials found a significant reduction in HbA1c levels in favour of the intervention group (Ferguson et al, 2015). Conversely, a meta-analysis of eight randomised clinical trials found no significant changes in the mean HbA1c levels between the participants in the educational intervention and those receiving usual care, which coincides with the present study (Cunningham et al, 2018).
An important aspect that must be analysed is the base value of the HbA1c levels. The participants in the present study had means HbA1c levels within the control range, but other studies in the scientific literature were conducted in people with poor glycaemic control. Thus, a greater benefit can be expected from the educational interventions for self-control of diabetes and, consequently, decreased HbA1c levels (Chrvala et al, 2016; Cunningham et al, 2018).
Furthermore, it has been determined that educational interventions are more effective when offered by the interdisciplinary staff compared with a single provider and, regarding the way of providing them, individualized interventions are more effective than group interventions, but combined interventions have greater effect (Chrvala et al, 2016; Cunningham et al, 2018).
The strengths of this investigation include a dropout rate of less than 20%. The sociodemographic and clinical characteristics of the groups at the beginning of the study were statistically similar, which indicates that the random assignment procedure was robust. SBP was measured objectively by using ambulatory blood pressure monitoring as a more reliable and accurate measure. Finally, advanced statistical methods were used for data analysis. However, the present study has some important limitations to consider as well. Since the clinical trial was of the parallel type, the findings could have been compromised as a result of physicians involved in the usual care treating patients in both arms of the study, something that could have been avoided had a cluster design been used. Similarly, the Hawthorne effect cannot be neglected, which implies a modification in some aspect of the participants' behaviour as a consequence of their knowing that they are being studied and not in response to some type of manipulation contemplated in the intervention (Sharpe et al, 2019). The means SBP and HbA1c were within optimal levels at the baseline, which is why significant changes were not observed at the 12-month follow-up, especially the HbA1c levels. It is also likely that the study did not have the adequate power to detect the calculated delta difference in SBP and HbA1c between the groups at the 12-month follow-up. Lastly, timely delivery of pharmacological treatment was not documented by the health system during follow-up, an aspect that is vital for disease control.
Implications for clinical practice and future research
This study suggests that the individual teaching intervention delivered by nurses via a multifaceted approach can be effective in improving therapeutic adherence and control of SBP in individuals with diabetes and/or hypertension. Since minimal changes were observed in HbA1c levels, further studies are needed to include patients with poorly controlled diabetes.
Moreover, given that the intervention addressed different aspects (diet, physical activity, pharmacological treatment, etc.) suggested by clinical management guidelines for hypertension and diabetes, it could be enhanced by other members of the multidisciplinary team, such as pharmacists, dietitians and physiotherapists. Thus, in the long term, sus interventions could be incorporated in daily practice as part of comprehensive care for people with cardiovascular risk factors.
KEY POINTS
- Educational interventions that use strategies with a multifaceted approach have turned out to be more effective to improve adherence to treatment
- Interventions led by nurses and in collaboration with other members of the health team have shown to improve adherence to treatment
- The nursing-led multifaceted individual teaching intervention has been effective in improving adherence to the therapeutic regimen and in the short term reducing SBP in people with hypertension and T2DM
- This intervention did not achieve significant changes in HbA1c levels, more studies are needed that include uncontrolled patients, with HbA1c values above the control range
CPD REFLECTIVE QUESTIONS
- How to implement an individual teaching intervention led by nursing in the improvement of adherence to the therapeutic regimen from a multicomponent approach in people with hypertension and T2DM is a more realistic scenario?
- What is the cost of implementing an individual teaching intervention led by nurses in improving adherence to the therapeutic regimen from a multicomponent approach in people with hypertension and T2DM?
- What are the long-term benefits of individual teaching led by nurses in improving adherence to the therapeutic regimen from a multicomponent approach in people with hypertension and T2DM?


