Community nurses working in palliative care encounter death as part of their work. With the COVID-19 pandemic, community nurses are exposed to more deaths than before, and this can be argued to have an adverse impact on their own wellbeing and ability to continue providing such care. Death and dying episodes among patients tend to have an negative impact on palliative care professionals (Nicol and Nyatanga, 2017). By extension, the reactions and experiences of relatives and those deemed important to the patient are also witnessed by community nurses, with a negative impact on their caring. For families and close friends, grief tends to follow the knowledge of the loss (whether it be impending or has happened), and community nurses are ever present to support them. The argument here is that the same health professionals might experience a sense of loss as well, and, therefore, grieving would only be natural. Nicol and Nyatanga (2017) explained how health professionals forge caring relationships with their patients, and through this, they become emotionally attached to form affectionate bonds (Bowlby, 1987). The advent of death breaks this attachment and results in feelings of grief. Most literature on loss, including Stroebe and Schut (1999) and Bowlby (1987), claims that affectionate bonds are formed as people develop relationships with each other. The claim is that, the closer or stronger the relationship, the deeper are the emotional affectionate bonds between people. It also translates that, when death occurs to one person in the relationship, those left behind (the bereaved) experience great pain. The logical point from this is that health professionals often develop relationships with their patients and, therefore, experience loss and grief; they also enter into bereavement following the death of their patients. In fact, they might have multiple bereavement episodes and concurrently, too, as they are exposed to more deaths, some resulting from COVID-19.
Supportive strategies
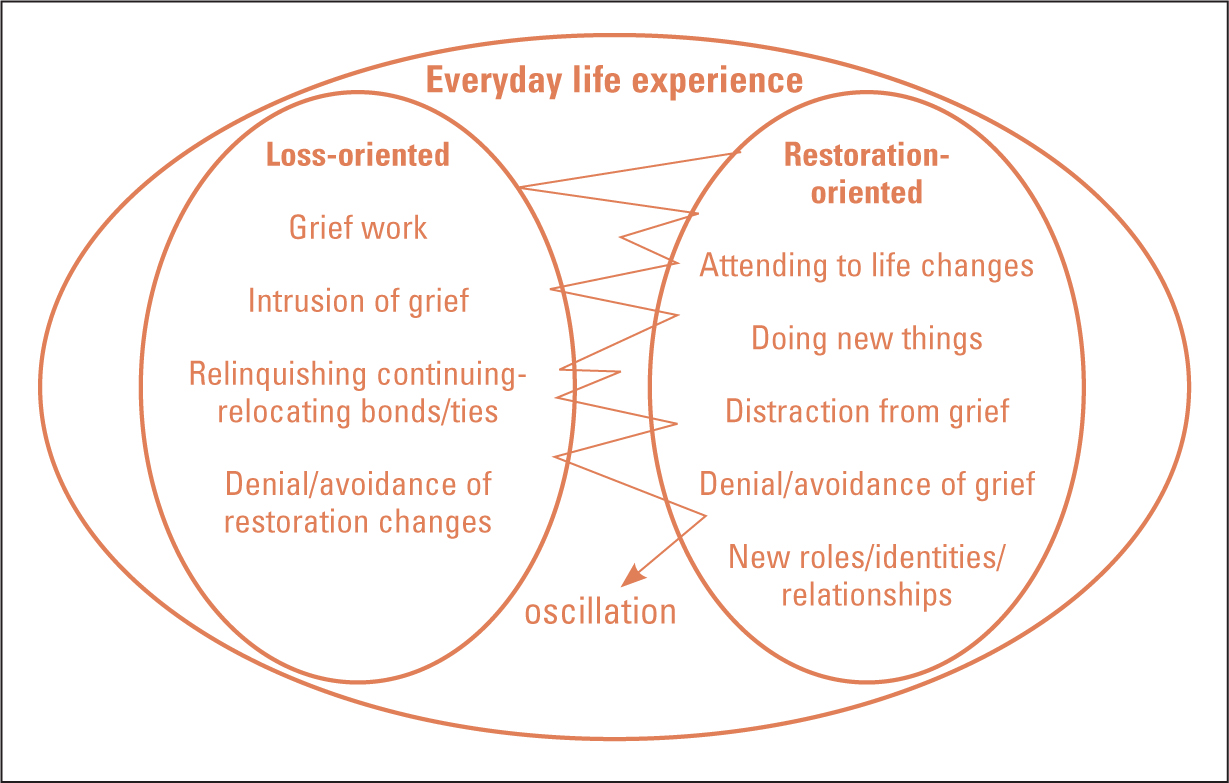
The literature is full of strategies for supporting families during and after death. For example, one modern approach is the dual process model for coping in bereavement developed by Stroebe and Schut (1999), which acknowledges the loss, but is forward looking in its support for the bereaved. First, the model recognises two important theories that many bereaved individuals experience:
Here, people use denial in a positive way (although it is unfortunate that it is referred to negatively, as denial), as they are literally taking time out to reorganise, compose and refocus themselves and find new energy to grieve. Thus, this time out (referred to as denial) is, in fact, quite positive in helping the bereaved adjust and face up to life without the deceased. The challenge is how much time out is positive, before it becomes a drawback.
Letting go is the idea of somehow relinquishing everything about the deceased so that the bereaved can move on with their life. The dual process model helps to recognise these issues and rightly addresses them by creating a dynamic process that encourages the bereaved to oscillate between different emotions. The oscillation is between loss-oriented emotional states and restoration-oriented tasks of everyday life activities. This is seen as a perfect balance for grieving and moving on with life, both at the same time. The oscillation time is also important, in that the bereaved can clear their mind as they move from one phase to another, as demonstrated in Figure 1. Although these strategies are meant for families, community nurses could also apply them to manage their own experiences with dying and deceased patients.
Stroebe and Schut (1999) made an interesting observation about gender differences by claiming that most women are loss-oriented while men are restorative-oriented in coping with death. It can, therefore, be concluded that women may take long to grieve and bereave their loved ones. The implication from this should draw attention to finding better and extra ways of supporting women who are bereaved.
However, a bigger challenge is that, while the dual process model might help relatives cope, no such model exists for health professionals who (as argued above) may experience similar losses and grief. Nursing is predominantly a female profession, which is also reflected in community nursing, which means that these individuals may take longer to process and manage their own feelings of loss and bereavement.
Conclusion
Community nurses are at the centre of providing palliative care in patients' homes. The increase in the number of deaths due to COVID-19 has multiple impacts on community nurses' wellbeing and care delivery. Therefore, more caring support is needed for community palliative care nurses. Community care services should have an established protocol or ritual following patient death, and this should be communicated to all professionals, so that they can access it when the need arises.

