Since the inception of the NHS 70 years ago, the pressure to deliver high quality, accessible public healthcare while generating efficiency savings has never been a more pressing and topical issue. The UK has an increasing ageing population, with 20.2% of the population predicted to be aged 65 years and over by 2027 (Age UK, 2018; Office for National Statistics, 2018). Urinary incontinence is known to increase in prevalence with older age (Gibson et al, 2016). Therefore, it can be assumed that the number of community patients requiring input from continence nurse specialists is set to increase, as are the number of prescriptions for continence appliances. This increase in continence prescribing was previously evidenced in 2007/08, when prescribing for continence products increased by 5.2%, compared to 0.45% for overall prescribing (Mangnall et al, 2010).
With this predicted future increase in prescriptions for continence appliances, the effective management of such prescriptions will be essential. Correct management will ensure patients are not being over-prescribed devices that could potentially go to waste, with associated financial implications. This article introduces a new product—Ugo 4 Weeks—that has been designed to enhance stock management of catheter drainage and fixation devices by providing a 4-week supply of products within a single box. It can benefit patients living with both short-term and long-term urinary catheters and provides generous cost savings compared to prescribing appliances individually.
It is estimated that there are 14 million people in the UK living with bladder dysfunction and 6.5 million experiencing bowel dysfunction (McShane, 2015). Complications of incontinence, such as urinary tract infections (UTIs), catheterisation and faecal impaction, can lead to hospital admission for extended lengths of stay (NHS England, 2018). The importance of monitoring these patients in the community setting is crucial, as it is known that early intervention can have a positive impact on patient outcomes (British Medical Association (BMA), 2017).
Catheter-associated urinary tract infections (CAUTIs) have significant associated costs of additional bed days and treatment for patients who are admitted to hospital, and this is estimated to cost the NHS up to £99 million per annum, or £1968 per episode (All Party Parliamentary Group for Continence Care (APPG), 2015). Despite this significant cost, urinary catheters are still being inserted in the acute setting when not clinically indicated. Nearly one-third of urinary catheter-days are inappropriate in medical and surgical inpatients, with 26% of catheters inserted in emergency department settings having no appropriate indication (NHS England, 2018). It is also known that there is a 5% increase in the likelihood of a patient developing CAUTI each day a urinary catheter remains in situ (Taha et al, 2017). This is further confirmed by Ansell and Harari (2017), who stated that ‘the longer a catheter remains in situ, the more likely the patient is to require increasing input from NHS services to respond to both planned and unplanned interventions.’ This highlights the importance of urinary catheters being reviewed regularly and removed promptly when appropriate. Despite this, there are still 90 000 people living in the UK community with a long-term, indwelling catheter (Ansell et al, 2017), and it is essential that catheter drainage and fixation prescriptions for this patient group are managed effectively.
Inappropriate prescribing of continence products
Early assessment by a qualified and appropriately trained professional allows a patient-centred and cost-effective care pathway to be followed, leading to better outcomes (APPG, 2011). In clinical practice, it is not unusual for continence assessments to be delivered in an inconsistent manner (Wagg, 2009). Patients may be prescribed urology or bowel appliances by a medical practitioner for many years without review. This can result in inappropriate or unnecessary prescribing of products (Orrell et al, 2013).
According to Mangnall et al (2013), some patients have concerns over having items incorrectly prescribed, incorrect products being dispensed and delays in their prescription being issued from the GP surgery. These concerns can lead to stockpiling, as the patient feels the need to store products ‘just in case’.
Another contributing factor identified by Mangnall et al (2013) is GPs not having sufficient in-depth knowledge of the products available to make effective prescribing decisions. The United Kingdom Continence Society's (UKCS) (2015) Minimum Standards for Continence Care Module 4 states that ‘health professionals should be able to demonstrate knowledge of available and suitable products for managing urinary incontinence and be able to counsel patients about their correct use.’ Continence nurse specialists acquire in-depth, up-to-date product knowledge in their roles, so it could be argued that they are best placed to make recommendations on appropriate product selection and usage.
Commissioning of continence services
Harari et al (2013) found that continence nurse specialist referrals are rising nationally, while budgets are decreasing and costs for appliances and management products continue to rise. The increasing burden of an ageing population combined with limited resources has led local clinical commissioning groups (CCGs) to consider different, innovative ways of working to commission continence services locally.
The Commissioning for Quality and Innovation (CQUIN) framework was introduced to support improvements in service quality and the development of better patterns of care (NHS England, 2014). There are now three CQUINs relating to bladder and bowel service provision. These are:
The APPG (2011) stated that care provided within integrated continence specialist advisory services helps to improve patients' clinical outcomes, reduce unplanned hospital admissions and improve patient experience, as well as offering value for money, with direct visible cost savings. These services also aim to identify patients whose care needs to be escalated, helping to prevent them escalating up the prevention pyramid (Figure 1).
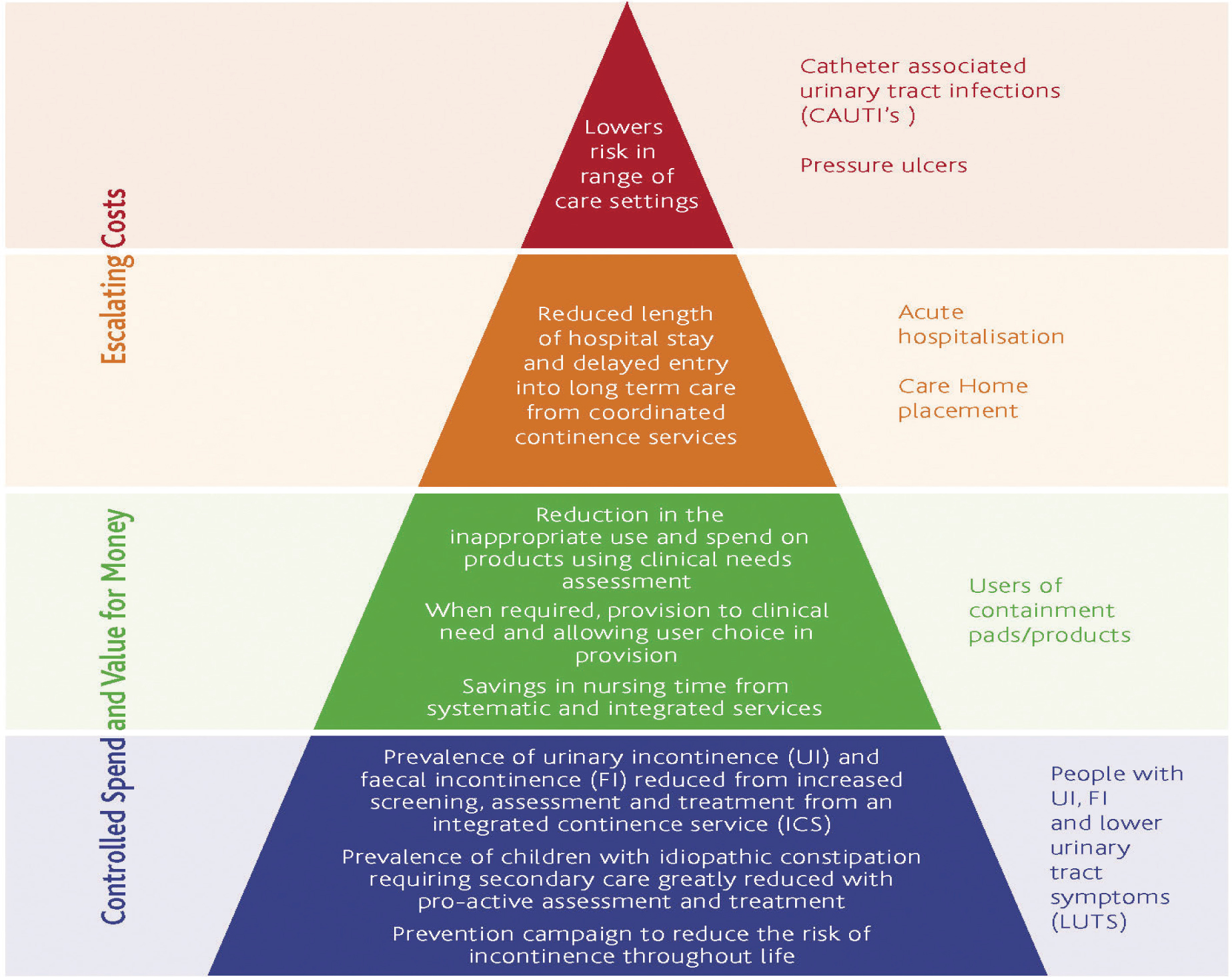
Using a pre-emptive approach can help to reduce admissions and costs for the treatment of continence-related conditions, such as UTIs, the cost of which averaged £2.1 million per CCG in 2012/13 (NHS England, 2018).
Evidence supporting the impact of continence nurse specialist intervention
In a randomised-controlled trial conducted in the Netherlands, Albers-Heitner (2011) established that interventions by continence nurse specialists resulted in improved speed and convenience of access to medicines and appliances, both of which were identified as key benefits of nurse prescribing by patients. Cost-saving efficiencies of 58% were also estimated as a result of continence nurse specialist input, as well as a significant reduction in the severity and impact of incontinence after a 3-month period. Creedon et al (2015) cited that increasing the number of nurse prescribers has a twofold effect: improving patient access to services and relieving pressure on doctors, thereby preserving limited medical resources for seriously ill patients.
These benefits were demonstrated in southeast Hampshire after the introduction of a continence prescription service, which in its first year led to a 45% reduction in the number of out-of-hours contacts involving patients using the continence service (from 24 to 13) and a 25% reduction in hospital admissions (from 27 patients to 20). Further, this service significantly reduced the workload of GP practices in the area, which otherwise would have been responsible for issuing prescriptions for approximately 2000–2500 patients (South Eastern Hampshire CCG, 2017).
Making appliance users more visible to continence nurse specialists
Having a centralised catheter caseload under the care of continence nurse specialists facilitates case finding and makes high-risk CAUTI patients more ‘visible’ to the continence nurse specialist. When the patients or their carers ring to order more catheter appliances, they are asked several trigger questions that will highlight if they are experiencing any issues with their catheter, such as UTIs, bleeding, trauma or frequent blockages. This brings the patient to the attention of the duty nurse prescriber, who will review their clinical record and troubleshoot, discuss and agree a plan of care with the patient, carer or community nurse. This early intervention and clinical review prompts a pro-active, evidence-based catheter care approach (Royal College of Nursing (RCN), 2019).
Accessing continence and appliance support
A nurse-led prescription service can assist with correcting issues regarding product usage. For example, male patients who use external urinary sheath drainage systems can sometimes experience fitting issues, leakage problems and skin issues. When carers are ringing to order more sheaths and these are not due, the continence nurse specialist can offer clinical and practical support to the patient to troubleshoot any issues around fitting the sheath and make different brand recommendations if necessary, instead of continuing to prescribe an ineffective and inappropriate sheath. A clinical review may result in re-measuring or basic information sharing with the patient and/or carer around the correct application of sheaths.
Streamlining continence product prescribing and reducing waste
Common issues with continence product usage involve incorrect product use by patients and/or carers. For example, breaking the closed drainage system by unnecessarily disconnecting the catheter leg bag from an indwelling catheter inadvertently increases the risk of infection (Wilson, 2015). Some patients may also use more catheter leg bags than necessary, which also increases the risk of infection. By engaging with the patient and, if necessary, the community nurse, the continence nurse specialist can identify any inappropriate catheter care practices and use their knowledge and expertise to implement corrective action. If such concerns are being flagged to a nurse-led prescription service from care home groups, this can trigger safeguarding concerns in relation to poor catheter care and highlight a requirement for additional training and support for care home staff.
When managing a large caseload of patients with catheters, it is essential that appliance stock levels are carefully monitored, to ensure any unusual or unnecessary prescribing practices are highlighted and addressed. Ideally, stock levels should be appropriately maintained, so patients have a sufficient quantity to last until their next prescription review, but not an excessive quantity that could lead to stockpiling and product wastage. However, this does not always occur in reality.
Ugo 4 Weeks
As a solution to the issues mentioned above, a new, innovative product has been developed, which is purpose designed to streamline the prescribing process for catheter drainage and fixation supplies. Ugo 4 Weeks is a 4-week urinary drainage and management system designed to provide all the catheter drainage and fixation devices a patient needs to last a 4-week period, all included within one box, on a single prescription with one dispensing fee (see Box 1 for product contents). This system helps reduce unnecessary wastage of product and highlights issues with incorrect product usage. For example, the quantities provided in Ugo 4 Weeks should last a 4-week period, and if more leg bags are being requested in this time, it may indicate that they are being changed too frequently.
The four Ugo Fix Gentle catheter clips included in each Ugo 4 Weeks box provide effective fixation at the bifurcation of the catheter (the port where the catheter connects with the leg bag). The soft, skin-friendly silicone technology makes them comfortable to remove and reposition, and they are safe for use on the delicate skin of older people. In addition to using the products included in each Ugo 4 Weeks box (Figure 2), patients can use add-on catheter fixation devices in a size best suited to them, such as catheter straps (i.e. Ugo Fix Catheter Strap) and leg bag sleeves (i.e. Ugo Fix Sleeve leg bag holder).

All catheter users in the community using Ugo 2L Drainage Bags (included in Ugo 4 Weeks) are eligible to receive a complementary Ugo Stand with Dignity. This bag stand has been designed with discretion in mind and features a removable cover, so the individual has the choice of having the 2-litre bag visible or not.
If prescribed separately, catheter drainage and fixation supplies are packaged in separate boxes. Therefore, by providing all of these devices within a single box, Ugo 4 Weeks presents a more environmentally friendly option.
The patient has been a central consideration in the design of the Ugo 4 Weeks box. It features a discreet design, which makes it ideal for convenient storage in patients' bedrooms or bathrooms.
Differing box quantities for products ordered individually
Many catheter drainage and fixation supplies are provided in boxed quantities designed to last differing lengths of time, and this can make re-ordering a challenge. For example, leg bags are typically provided in a box of 10, and this volume of product should last for 10 weeks. Some fixation devices are provided in boxes of four, with the volume of product designed to last for up to 4 weeks. Juggling varied pack sizes means there is a possibility of either ordering too much product, which then potentially goes to waste, or ordering too little, with the patient then requiring an emergency prescription. This can be difficult to manage, particularly where a caseload of multiple patients with catheters is concerned. Ugo 4 Weeks is ideal for use in these scenarios, making re-ordering more convenient for clinicians to manage and also giving patients peace of mind that they will not run out of the contained products. With only one code to remember per Ugo 4 Weeks box, the re-ordering process is also simplified.
Ugo 4 Weeks for short-term catheterisation
For patients only requiring a urinary catheter for a short period of time and due to receive a trial without a catheter (TWOC), the quantities provided in each box of Ugo 4 Weeks are ideal. There is less appliance wastage and greater cost savings when compared to prescribing a catheter leg bag box containing a 10-week supply of bags. The same applies for patients with catheters who are receiving palliative care, where it is anticipated they will be progressing towards end of life within the following month.
Ugo 4 Weeks in the care home environment
In the authors' experience, it is not uncommon for care home staff to routinely request repeat prescriptions without physically checking their patients' stock levels. This could occur for a variety of reasons, such as staff not having time to complete a stock check or agency staff not being familiar with each residents' individual product requirements. Routine repeat prescribing can result in over-stocking and higher prescribing costs. Ugo 4 Weeks allows care home staff to keep track of each residents' stock levels with ease and in a way that is not time consuming. It also highlights to the continence nurse specialist instances of incorrect product usage and where clinicians could benefit from further training.
Cost savings with Ugo 4 Weeks
There are cost savings available when prescribing Ugo 4 Weeks for patients with both short-term and long-term urinary catheters. Table 1 demonstrates the savings made available in Nottingham, using pricing data based on the most frequently prescribed products over a 4-week to 6-month period of catheter usage for a individual user. The scale of the available savings are considerable when multiplied across all catheter users in a given area.
| Product | Week 1 | Week 4 | Week 8 | Week 12 | Week 24 | |
|---|---|---|---|---|---|---|
| Leg bag | £26.53 | £0 | £26.53 | £0 | £26.53 | |
| 2L drainage bag | £10.32 | £10.32 | £10.32 | £10.32 | £10.32 | |
| Catheter fixation | £14.68 | £14.68 | £14.68 | £14.68 | £14.68 | |
| Leg bag straps | £12.88 | £0 | £12.88 | £0 | £12.88 | |
| Total cost of prescribing | £64.41 | £25 | £64.41 | £25 | £64.41 | |
| Rolling cost of prescribing the above: | £89.41 | £153.82 | £178.82 | £332.64 | ||
| Ugo 4 Weeks | £29.41 | £29.41 | £29.41 | £29.41 | £29.41 | |
| Rolling cost of prescribing Ugo 4 Weeks: | £58.82 | £88.23 | £117.64 | £205.87 | ||
| Cost difference (prescribing products separately vs. prescribing Ugo 4 Weeks) | £35.00 | £30.59 | £65.59 | £61.18 | £126.77 | |
| Percentage cost savings available with Ugo 4 Weeks | 54% | 34% | 43% | 34% | 38% |
There are also cost savings available on prescription costs, as each box of Ugo 4 Weeks can be issued on a single prescription. Ugo 4 Weeks features on Part IXB of the Drug Tariff and has a dispensing fee of £3.40, making it significantly more cost-effective compared to incurring dispensing fees for prescribing each contained product individually. Table 1 shows individual product costs based on these items being ordered only when they are needed. However, products prescribed individually are provided in different boxed quantities. This can lead to more products being ordered than what is required at the time and increases the risk of excess products going to waste. Taking this into account, the individual product costs in Table 1 are likely to be higher in reality.
Supportive literature
In addition to catheter drainage and fixation supplies, each Ugo 4 Weeks box contains informative patient and carer user guides. These explain how to apply, care for and remove the enclosed products. These user guides can serve as a helpful and reassuring point of reference for community patients between nurse visits, helping to reduce community nurse call outs. They can also be used as an educational tool by clinicians to provide further information to patients and carers about the products being used and their indications.
Case studies
Case study 1: a patient on a short-term catheter awaiting a TWOC
An 83-year-old man with a diagnosis of dementia was admitted to hospital and treated for an upper respiratory tract infection. He was catheterised on admission for acute urinary retention. He had had a previous diagnosis of a benign enlarged prostate and was prescribed finasteride and tamsulosin for many years. Prior to this recent admission, he was managing his urinary incontinence using a sheath and did not have any significant bothersome lower urinary tract symptoms. He was discharged home with an indwelling urethral catheter. When his wife rang the continence prescription service to order more catheter appliances, she had a conversation with the continence nurse regarding his catheter care needs. After this review of his clinical need for the catheter, it was agreed that the patient would receive a TWOC at home 2 weeks after discharge.
Ugo 4 Weeks was prescribed so that the patient would have adequate interim supplies until the TWOC was undertaken. If his catheter drainage and fixation supplies were prescribed individually and the TWOC was undertaken successfully after 2 weeks, a significant volume of the products would have been wasted. For example, most leg bags come in a box of 10. The use of Ugo 4 Weeks for 2 weeks resulted in the wastage of only two leg bags. In comparison, if the patient were prescribed the products individually, eight leg bags would have been wasted. Following the TWOC, the patient was able to resume using sheaths. The clinical review by the continence nurse specialist prompted arrangements for the TWOC in partnership with the district nurses and led to the removal of his catheter, which reduced his risk of CAUTI and improved his quality of life.
Case study 2: long-term catheterised residents in care homes
Following several requests from nursing staff at a care home for leg bag repeat prescriptions that were not due, the duty continence nurse prescriber rang the care home to request that staff undertook a thorough stock inventory, and also discussed catheter care provision for their residents. Following discussions with the staff, it became apparent that some clinicians were performing prophylactic catheter irrigations on residents without any clinical rationale for doing so. This routine practice of performing catheter irrigation as part of a blockage prevention strategy, regardless of whether or not the catheters were blocked, increased the risk of sepsis to this group of residents. This in turn raised safeguarding concerns around the clinicians' knowledge, training and competence regarding best-practice catheter care interventions.
The continence nurse collaborated with the care home manager to implement an immediate safeguarding plan and conducted a review to ensure that all nursing staff involved in catheter care provision attended immediate catheterisation update training programmes. Ugo 4 Weeks assists in highlighting any ordering inconsistencies at an earlier stage than if patients were prescribed their devices in individual boxes. Another benefit in the care home environment is having each residents' supplies contained within a single box. This increases feelings of ownership, which can reduce the likelihood of staff borrowing products to use for other residents, when they should in fact only be used by the individual whose name is on the prescription.
Case study 3: a patient with a catheter receiving palliative care
A 46-year-old woman was discharged home, as she was approaching end of life. The patient was continent but bed-bound and required hoisting. She was unable to use a bed pan or commode, as this caused extreme discomfort. The patient had capacity and was adamant that using continence pads was not an option, as this would negatively impact her self-esteem and dignity. She had specified in her advance care plan that it was her preference to be catheterised when she reached end of life. A Ugo 4 Weeks box was prescribed to provide sufficient but not excessive volume of stock, considering her prognosis.
Conclusion
It is clear that nurse-led continence prescription services deliver numerous benefits. Significant cost savings can be made by CCGs by effectively managing continence product prescriptions. More regular patient evaluations and appliance review interventions can be facilitated by transferring the prescribing responsibility for continence appliances from GPs to continence nurse specialists within nurse-led prescription services.
Using products that support streamlined prescribing, such as Ugo 4 Weeks, clearly highlights to clinicians any issues with incorrect product usage. This can assist in triggering early intervention from a continence nurse specialist and potential avoidance of harm by allowing them to share best-practice catheter care with the patient or community nurse. Ugo 4 Weeks can benefit both short-term and long-term catheter users. It promotes correct product usage, reduces unnecessary appliance wastage and provides a simple and efficient solution to catheter drainage and fixation management, helping to generate significant cost savings.

