Delegation of medicines administration from a regulated health professional such as a registered nurse (RN) to a healthcare support worker (HCSW) is practised in community settings in a range of countries (Shore et al, 2022). In this article, a HCSW (such as a healthcare assistant or an assistant practitioner), is an employee providing healthcare support, usually as part of a community nursing service provider. Healthcare can also be delegated to care workers in social care. Recent guidance on delegation in health and social care defines a delegated healthcare intervention as ‘a health intervention or activity usually of a clinical nature, that a registered healthcare professional delegates to a paid care worker’ (Department of Health and Social Care (DHSC) and Skills for Care, 2023). Delegation should be embedded within person-centred care, in the best interest of, and in collaboration with the person receiving care (DHSC and Skills for Life, 2023).
As insulin is a high-risk medication, the Delegation of Insulin Administration (DIA) requires careful attention. It is anticipated that achieving a safe and supportive framework to guide DIA may help to facilitate the safe delegation of other medicines. The support of HCSWs in providing insulin injections has been reported as essential for managing demand at peak times in organisations with a high caseload of patients who cannot safely self-inject (Stenner et al, 2023). Although improving team efficiency in meeting demand is a top motivation for DIA, research indicates benefits in terms of timely access to medicines for patients, service efficiency, improvement in team working, plus benefits for HCSWs related to career progression and job satisfaction (Owen, 2009; Cook, 2015; Dutton et al, 2018; Gregory, 2019; Castro, 2021; Stenner et al, 2023).
Delegation should occur within a framework of local governance that includes training of HCSWs, assessment of their competencies (usually by RNs) and adherence to protocols that maintain patient safety (Castro 2021; Shore et al, 2022; DHSC and Skills for Life, 2023). Research also points to the role that governance has in building confidence and acceptability of DIA for staff and service users (Stenner et al, 2023). Dedicated time and resources are needed to set up DIA in an organisation, including time to engage key stakeholders (Cook, 2015; Cradock, 2023). In 2020, the voluntary framework for the delegation of insulin administration was launched to provide support for organisations. Commissioned by NHS England, and in collaboration with Diabetes UK, the framework was developed with input from stakeholders, an expert working group and eight national exemplar sites (Diabetes UK). It includes supporting guidance, sample policy templates, documents and checklists, along with a series of recorded webinars featuring exemplar sites presenting how they set up and supported DIA. The resources are freely available on the Diabetes UK website. Plans to rollout the framework were paused due to the COVID-19 pandemic and escalated late 2022 and early 2023 with the support from NHS England with a community nurse clinical fellow.
This paper reports on a survey of the uptake and use of DIA in England and the use of the guidance.
Aim and study design
The study aim was to evaluate use of the national voluntary framework for the delegation of insulin administration and the uptake of this delegation practice in community nursing in England.
Objectives
- To establish the extent of roll out of delegation of insulin administration in community nursing teams in England and describe key characteristics of initiatives
- To evaluate awareness of and use of the voluntary framework for the delegation of insulin administration
- To identify key barriers and facilitators to the delegation of insulin administration
- To identify support needs for those involved in delegation.
A cross-sectional online survey was designed with input from a broad project management group (including patient representatives, clinical leads, diabetes specialists, delegation experts, medicines management specialists and community nursing leads) and piloted on 12 volunteers. A mix of closed and open-ended questions covered: service type, staffing, rates of insulin administration, experience and practice around the delegation of insulin administration, benefits and challenges), resource awareness and use, and suggestions for further support.
There is a complex and evolving pattern of community health service provision in England, including NHS (acute hospital trusts, mental health trusts and standalone community health trusts) and non-NHS (social enterprises, private sector and community interest companies) organisations (The King's Fund, 2014). Recruitment was targeted at service providers, clinical leads or managers of community or integrated care services (ICS) providing insulin administration for adults with diabetes in England. As there is no national consensus on the number of these community nursing providers, we aimed to recruit a minimum of 100.
Invitations to participate in the survey were circulated on a range of social media platforms and networks relevant to community nursing services and diabetes specialist nursing. Recruitment occurred between November 2022 and March 2023. The survey was conducted by a team at the University of Surrey, commissioned by NHS England, and reviewed through the University of Surrey ethics committee assessment process (Reference number: 904570-904552-98669547).
Results
Characteristics of responding services
A total of 115 respondents completed the survey, representing each of the seven NHS regions in England. The major ity of responding organisations were NHS providers (n=96, 83%) and included a range of organisational types, including secondary care trusts, community and integrated trusts and community interest initiatives (Table 1).
Table 1. Characteristics of responding services
| n | % | |
|---|---|---|
| Provider | ||
| NHS organisation | 96 | 83.5 |
| Community interest group/company | 6 | 5.3 |
| Social enterprise | 5 | 4.3 |
| Adult social care provider | 3 | 2.6 |
| Independent sector provider | 1 | 0.9 |
| Other (GP practice) | 1 | 0.9 |
| Missing | 3 | 2.6 |
| Organisation type | ||
| Secondary care trusts | 33 | 28.7 |
| Community trusts | 20 | 17.4 |
| Mental health services and integrated care | 12 | 10.4 |
| Unspecified NHS Trusts | 5 | 4.3 |
| Community Interest Initiatives (CIC), Community Partnership CICs | 4 | 3.5 |
| Missing | 41 | 35.7 |
| Geographical location (NHS region) | ||
| North East & Yorkshire | 29 | 25.2 |
| Midlands | 17 | 14.8 |
| East of England | 16 | 13.9 |
| South West | 15 | 13.0 |
| North West | 13 | 11.3 |
| South East | 12 | 10.4 |
| London | 8 | 7.0 |
| Missing | 5 | 4.3 |
| Respondent job titles | ||
| Lead nurses, clinical leads, charge nurses, sisters | 36 | 31.3 |
| Service management and senior and team level | 20 | 17.4 |
| Community matrons | 18 | 15.7 |
| Community or district nurses/sisters, nurse practitioners, registered nurses, practice educators or developers | 18 | 15.7 |
| Diabetes specialists or consultants | 9 | 7.8 |
| Community nurse, specialists | 8 | 7.0 |
| Other | 2 | 1.7 |
| Missing | 4 | 3.5 |
| Delegation of insulin administration service | ||
| Yes | 93 | 80.9 |
| No | 21 | 18.3 |
| Missing | 1 | 0.9 |
| Aware of the National Framework | ||
| Aware | 58 | 50.4 |
| Unaware | 37 | 32.2 |
| Missing | 20 | 17.4 |
The composition of staff within services is shown in Figure 1 and Table 2. There was a total of 9148.2 whole time equivalent (WTE) staff reported across services, with a median of 23.7 (2.0–467.0) WTE per service. The largest staff group were community nurses at 53.0% (n=4850.6). Other non-registered staff (n=431.4, 4.7%) included administrative staff, logistical support workers, nursing associates, trainee nursing associates, patient educators, and diabetes care staff.
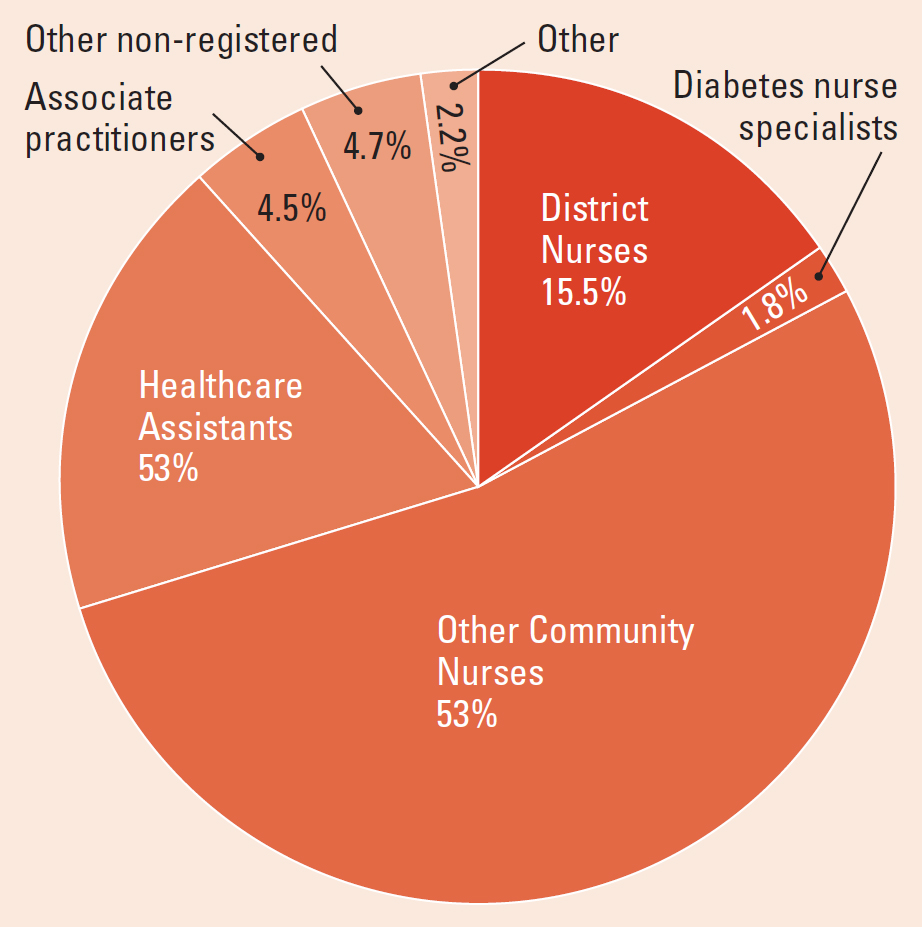
Table 2. Staff composition in community nursing services
| Number of FTE staff in services | ||||||||
|---|---|---|---|---|---|---|---|---|
| District nurses | Diabetes nurse specialists | Other community nurses | Healthcare assistants | Associate practitioners | Other nonregistered | Other | Total FTE staff | |
| Mean | 12.53 | 1.43 | 42.93 | 14.84 | 3.64 | 3.82 | 1.77 | 80.95 |
| SD | 19.93 | 3.28 | 71.55 | 21.49 | 6.86 | 28.32 | 9.64 | 105.88 |
| Median | 4.0 | 0.0 | 8.0 | 5.0 | 1.0 | 0.0 | 0.0 | 23.7 |
| Min | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 2.0 |
| Max | 111.0 | 19.0 | 325.0 | 100.0 | 50.0 | 300.0 | 100.0 | 467.0 |
| Total | 1415.76 | 161.98 | 4850.60 | 1676.60 | 411.78 | 431.38 | 200.06 | 9148.16 |
| % Total | 15.5% | 1.8% | 53.0% | 18.3% | 4.5% | 4.7% | 2.2% | 100.0% |
A mean of 118 (median: 59.0, standard deviation (SD): 145.7) insulin injections were administered per day across the sample, ranging from 1–600 per day.
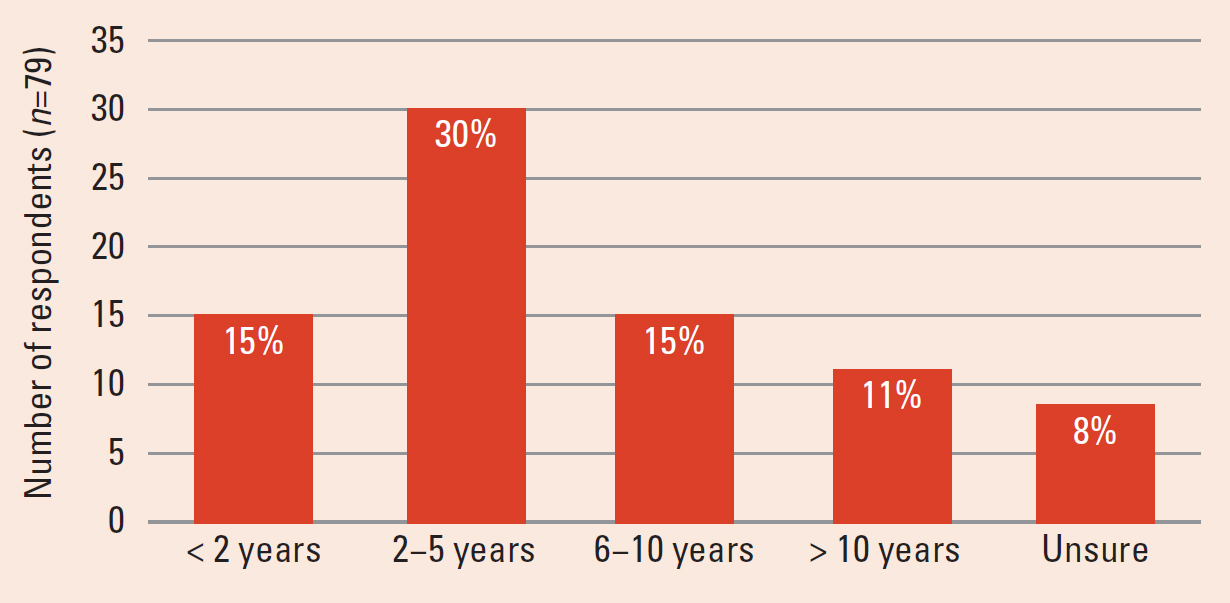
Delegation of Insulin Administration programmes
The majority (n=93, 80.9%) had delegation of insulin administration in place in their service. Of the 21 (18.3%) without DIA in place, around half (n=11, 52.4%) indicated an interest in future implementation of DIA, 8 (38.1%) indicated no interest and 2 (9.5%) did not respond to the question. Some 57% percent had started DIA within the past 5 years, whereas 33% (n=26) had been in place over 6 years (Figure 2).
Characteristics of Delegation of Insulin Administration
Most DIA training programmes were provided in-house (83.9%, n=78) and were either face-to-face (22.6%, n=26) or used a blend of online and face-to-face training (45.2%, n=52). To sign off on competency, RNs observed a minimum of 5.0 (range 1–20, mean: 5.9, SD: 4.0) insulin injections administered by HCSWs.
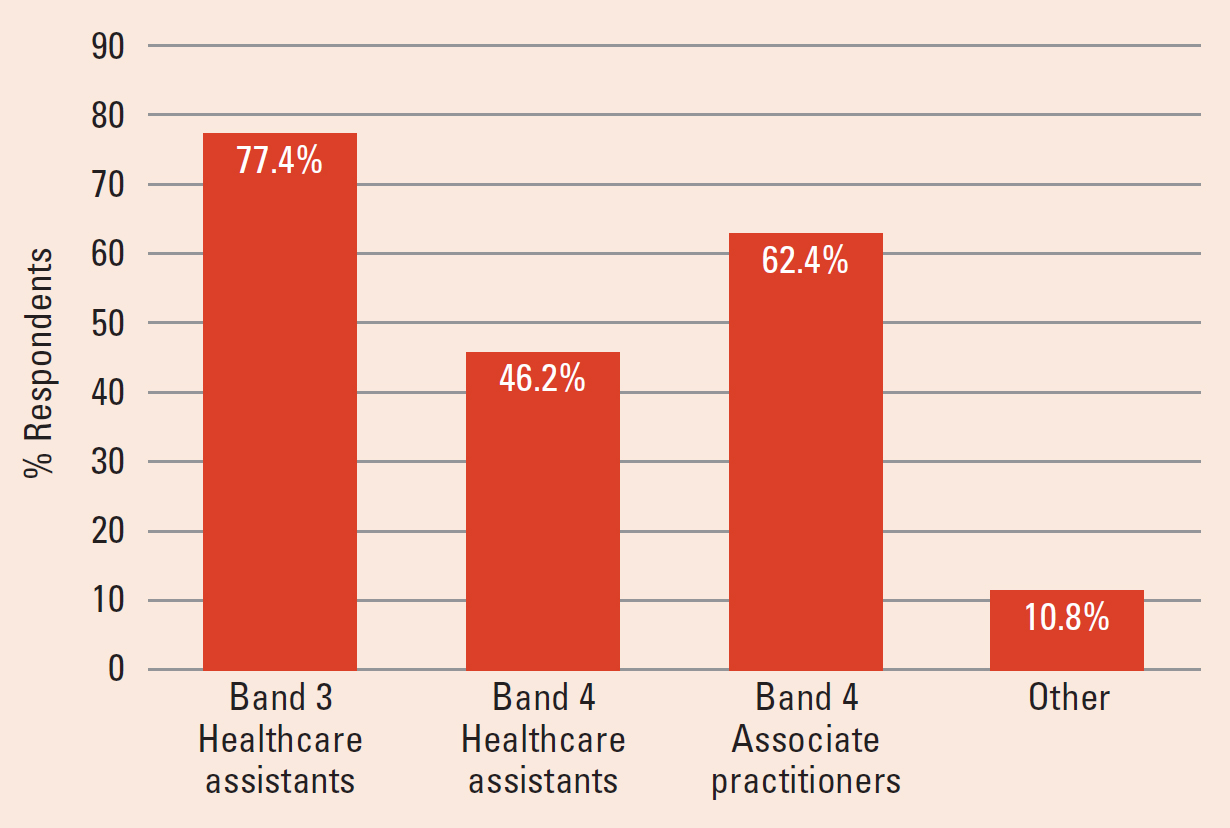
Services with DIA in place reported a higher number of WTE staff than services without DIA (median 30.0 versus 13.0, p=0.035) and administered a greater number of injections per day (median: 61.0 versus 21.0, p<0.036) than those without DIA. Insulin administration was delegated to Band 3 healthcare assistants (77.4%, n=72), Band 4 healthcare assistants (46.2%, n=43) and Band 4 associate practitioners (62.4%, n=58). Other staff (10.8%, n=10) were: nursing associates and trainee nursing associates, residential home carers and private healthcare assistants (Figure 3).
Provision of Delegation of Insulin Administration
Most services provided DIA in the client's privately owned or rented home (87%, n=81), or private residential or care home (81%, n=76). Half included council owned care homes (55%, n=51) and fewer provided DIA in nursing homes (16%, n=15) (Table 2). Adults over 65 years of age made up the largest proportion of recipients of insulin injections under delegation (88.2%, n=82). Recipients were mainly clients with type 2 diabetes, including adults (86.0%, n=80) and younger adults from 18 years of age (20.4%, n=19). However, clients with type 1 diabetes were also recipients: including adults (49.5%, n=46) and younger adults over 18 years of age (30.1%, n=28) (Table 3). Pen devices were most often used (n=81, 87%) although four services (4.3%) reported that vials and syringes were used to administer insulin under delegation.
Table 3. Settings and recipients of insulin administration by delegation
| n | % | |
|---|---|---|
| Settings where DIA occurs | ||
| Residents home (rented, owned, sheltered, retirement) | 81 | 87.1 |
| Private residential or care home | 76 | 81.7 |
| Council owned care home | 51 | 54.8 |
| Nursing home | 15 | 16.1 |
| Staff who administer insulin by delegation | ||
| Band 3 healthcare assistants | 72 | 77.4 |
| Band 4 healthcare assistants | 43 | 46.2 |
| Band 4 associate practitioners | 58 | 62.4 |
| Other | 10 | 10.8 |
| Client receiving insulin by delegation | ||
| Adults with type 1 diabetes | 46 | 49.5 |
| Adults with type 2 diabetes | 80 | 86 |
| Young adults > 18 years with type 1 diabetes | 28 | 30.1 |
| Young adults > 18 years with type 2 diabetes | 19 | 20.4 |
| Age group of clients receiving insulin by delegation | ||
| 18–24 | 28 | 30.1 |
| 25–40 | 36 | 38.7 |
| 41–64 | 63 | 67.7 |
| 65 + | 82 | 88.2 |
In services where DIA was in place, registered nurses continued to administer the largest proportion of insulin injections (mean: 76, median: 25 injections per day), Band 3 HCSWs administered a mean of 38.24 (median 17.5) injections per day and Band 4 healthcare assistants administered a mean of 11.84 (median: 4.0) injections per day (Table 4).
Table 4. Daily case load for insulin injections by staff group
| Registered Nurses | Band 3 HCSWs | Band 4 HCSWs | Other | Total | |
|---|---|---|---|---|---|
| Mean | 76.07 | 38.24 | 11.84 | 2.79 | 128.95 |
| SD | 101.61 | 65.03 | 20.74 | 14.24 | 161.61 |
| Median | 25.0 | 17.5 | 4.0 | 0.0 | 60.0 |
| Min | 1.0 | 0.0 | 0.0 | 0.0 | 1.0 |
| Max | 423.0 | 370.0 | 100.0 | 97.0 | 838.0 |
| Total | 5325.0 | 2677.0 | 829.0 | 198.0 | 9029.0 |
| % total | 58.9% | 29.7% | 9.2% | 2.2% | 100.0% |
Potential allocative value
Costs per working hour for different staff groups were obtained from the Personal Social Services Research Unit (PSSRU) Unit Costs for Health and Social Care report (Jones et al, 2022). Based on a 30-minute consultation time for DIA, which does not include travel time between consultations, we used unit costs for Band 5 RNs at £23 and HCSWs at £11.5. This is a conservative estimate for RN banding; however, the PSSRU only provide unit costs of a homecare worker in the social care sector which may not be representative of healthcare support worker unit costs. The difference in unit costs for band 5 RNs is £11.5, which when multiplied for the 3704 injections delegated per day across these services represents a difference of £42596 per day, and £15547540 per year for the whole sample. When divided by the number of services responding to this question (n=67), this is an average difference of £232052.84 per year, or £636 per day, per service.
These calculations do not take into consideration other costs, such as the cost of training, competency assessment and ongoing monitoring which offset these figures.
Benefits and challenges
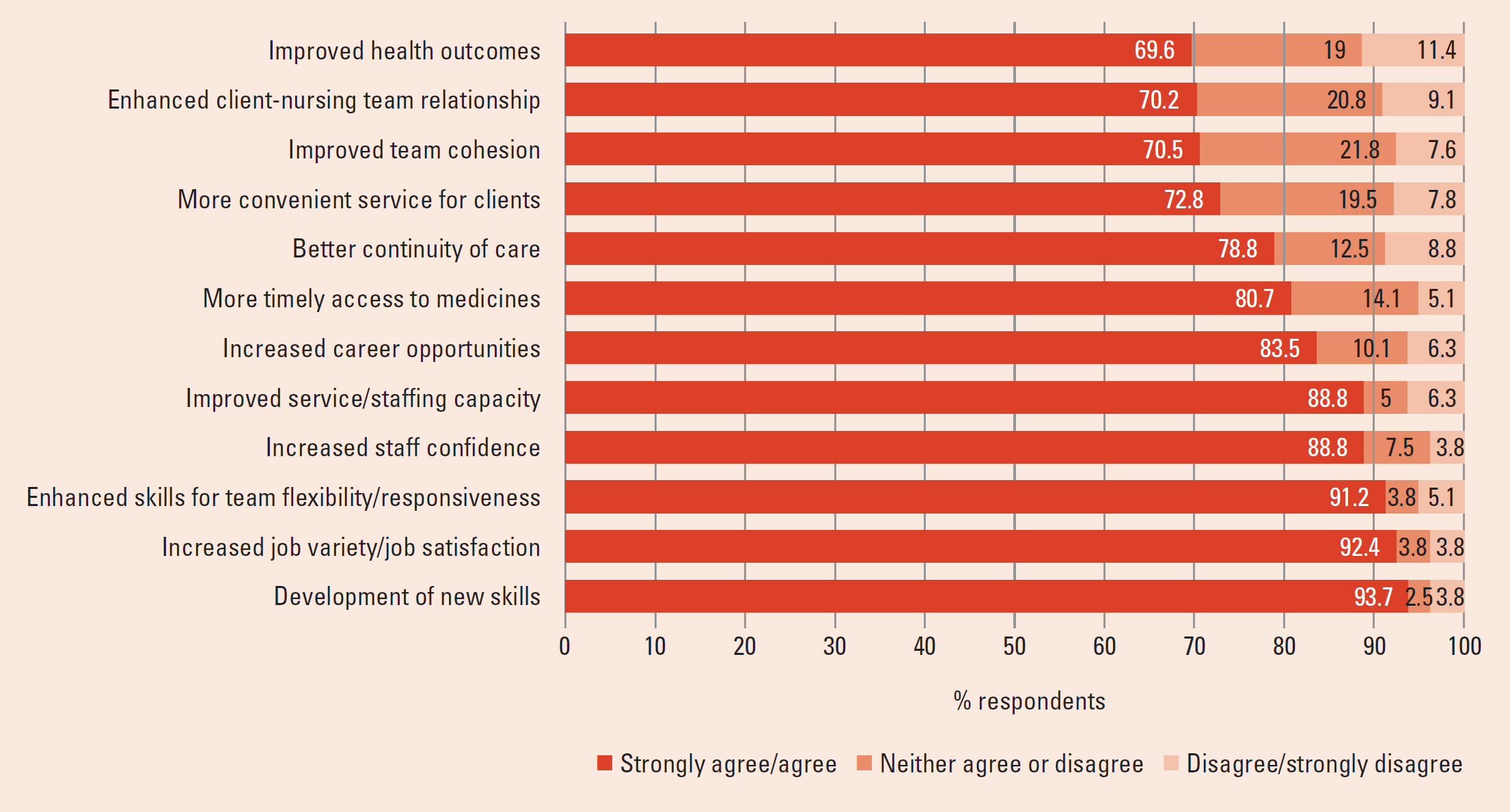
Respondents were asked to indicate the extent to which they agreed with 12 attitudinal statements concerning the benefits/advantages of DIA within their services (Figure 4). The majority agreed (69.6% to 93.7%) with each benefit. There were higher levels of agreement of benefit for HCSWs and staffing capacity than for aspects of patient benefit or team cohesion. Over 90% (n=84) strongly agreed/agreed that implementing insulin delegation developed new skills for HCSWs (93.7%, n=75) and increased job variety/job satisfaction (92.4%, n=74), with 91.2% (n=73) perceiving that it enhanced skill mix to improve the flexibility and/or responsiveness of teams. A total of 89% per cent (n=71) believed DIA increased confidence for HCSWs and improved service/staffing capacity. There was some uncertainty as to whether it improved team cohesion (21.8%, n=17) or client health outcomes (19.0%, n=15) as indicated by neither ‘agree’/‘disagree’ responses.
Challenges to DIA were reported as poor engagement from staff (including reluctance from some RNs and HCSWs) and care homes, large numbers of patients with complex conditions or insulin regimes who were not eligible for DIA, and the workload involved in setting up DIA, training, assessing and monitoring HCSWs.
Patient safety
Errors relating to DIA were reported to have occurred in 28 (30%) of the services. The three main error types reported in free text comments were:
- Dosing errors (e.g. administered wrong dose, wrong insulin, dose omission)
- Inappropr iate delegation (e.g. sliding scale insulin delegated)
- Failure to follow protocol/standard operating pre-administration checks, failure to escalate deterioration in patients condition).
Evaluation of resources and support needs
Half of all respondents (n=58) were aware of the national voluntary framework for DIA, mainly through word-of-mouth or the Diabetes UK website and webinars. Fewer of those without DIA in place (38.1%, n=8) knew about the framework. The majority found resources useful (81.3%, n=39) and of those who were not aware of the framework, 81% (n=30) considered national guidance for the delegation of insulin important. The framework and resources had informed existing DIA training programmes (35.0%, n=14), supported the development of a new programme (27.5%, n=11), or supported a case for developing DIA (15.0%, n=6). The framework had not been used by 15.0% (n=6) of services. Barriers to using the framework included already having DIA in place and lack of time/awareness to make use of it. Where difficulties had been encountered setting up DIA, these mainly focused on low engagement from care homes, along with insurance and liability concerns, workload pressures and managing the change process. Suggestions for further support for DIA included: providing a range of resources to support HCSW training, specific training tailored for care homes, and provision of national guidelines to support DIA, especially in care homes.
Discussion and conclusion
As far as the authors are aware, this is the first survey of DIA in England. Findings demonstrate that DIA is an established and valued initiative in community nursing services. Data show an expansion of DIA in the past 5 years, with more services intending to set up DIA, confirming the need for guidance in this area. There is growing awareness of the national voluntary framework for the DIA and services that have used this framework have found it helpful.
Findings demonstrate the important contribution of HCSWs in helping to provide insulin administration and releasing registered nurses' time to undertake more complex care. Services with a high caseload of patients requiring help with insulin injections were more likely to initiate DIA, supporting previous reports (Stenner et al, 2023) that improving service capacity at peak times is a key driver. Considerable cost differences were suggested; although these will be offset against the resources required to set up training, competency assessment and ongoing monitoring that are essential to the safe governance of DIA (Cooke, 2015; Cradock, 2023). However, improving service capacity is not the only motivation for DIA; findings reaffirm a range of previously reported benefits to patient care, HCSWs and teams (Owen, 2009; Dutton et al, 2018; Gregory, 2019; Castro 2021; Stenner et al, 2023). In addition to improved team flexibility and capacity, the strongest agreement was over benefits for HCSWs (skills development, job satisfaction and confidence) – benefits that may increase recruitment and retention.
This survey confirms most people receiving DIA are older adults with type 2 diabetes; however, just under 50% of services included adults with type 1 diabetes, including younger adults, and administration was not always via pen devices. As the voluntary framework covers DIA for people with type 2 diabetes, these aspects need further attention. Acceptance of DIA (by staff and patients) is often conditional on clear eligibility criteria (Stenner et al, 2023), such as being restricted to people with type 2 diabetes, stable blood glucose levels and non-complex treatment regimens. However, in some services, people with type 1 diabetes are eligible for DIA where local governance has been adopted for this case load of individuals (Castro et al, 2021).
Maintaining patient safety is a priority as findings demonstrate that errors do occur, reiterating the importance of initiatives to reduce insulin administration errors in this setting (Leeson, 2022). The predicted rise in diabetes with comorbidity (Sinclair et al, 2020), plus staff shortages (Care Quality Commission, 2022; Age UK, 2023), imply a continued need for delegation in which supporting safe practice is key. Patterns of delegation may change if community nursing caseloads become more complex and fewer people with diabetes are eligible for DIA. Staff mix configurations and patient caseloads are key factors considered by services when deciding whether to implement DIA and the introduction of the safer staffing tool is anticipated to facilitate workforce planning (Jackson, 2016).
Challenges to implementing DIA reveal a need for more guidance on best practice in the implementation process. It is known that using an inclusive team approach and involving staff at an early stage helps to address concerns about DIA, build trust and strengthen team cohesion (Castro et al, 2021; Shore et al, 2022; Stenner et al, 2023). Other suggestions made on the ‘10 tips for starting DIA’ (part of the voluntary framework resources) include factoring in time for staff discussion, holding joint training for RNs and HCSWs, and allocating funds for project management. Appropriately engaging with care homes to manage DIA was a challenge, particularly where there is high staff turnover (Cradock et al, 2023). It is timely that comprehensive guidelines to support delegation of healthcare to non-registered care workers in social care setting have recently been released (DHSC and Skills for Care, 2023). The translation of current knowledge to other settings and other medicines currently delegated will be invaluable to future work as it is important to build on good practice, lessons learnt to date and to highlight current gaps in knowledge.
Key points
- Delegation of insulin administration is expanding in community nursing services
- There are a wide range of benefits for staff and services (e.g. increased flexibility to meet demand, job variety and confidence of healthcare support workers) as well as for recipients (e.g. timely access to medicine)
- Challenges included engaging care homes to support delegation, improving patient safety, the complexity of care needs and the workload involved in setting up a delegation programme
- National guidance on delegation is welcome and is useful to services.
CPD reflective questions
- What policy and/or governance is in place in your service to support delegation of insulin administration?
- Have your local policies been reviewed against the national guidance on the delegation of insulin administration?
- What steps could be taken to avoid errors in relation to the administration of insulin?


