Working with service users in their home environment can be challenging for healthcare professionals in the community setting because of potential safety risks. These include household-related hazards (poor indoor air quality and toxic substances), healthcare risks (infection and environmental cleanliness) and security issues (violence and aggression, lone working) (Gershon et al, 2008; Vincent and Amalberti, 2016).
All of these risks are exacerbated by the unpredictable nature of providing healthcare at home, and the challenges of risk assessment and management in these circumstances. Despite this, the home environment remains an important and effective setting for acute and chronic healthcare provision in the 21st century, particularly because in the majority of cases, patients prefer home care and it is the policy focus of the Department of Health and Social Care (DHSC, 2023). Evidence-based strategies are needed to reduce risks and ensure that the home environment remains a safe and effective setting for healthcare provision.
Carbon monoxide poisoning is an important public health issue associated with mortality and morbidity. In 2020, a total of 116 deaths in the UK were attributed to carbon monoxide exposure (Office for National Statistics, 2021). There are approximately 4000 emergency department attendances and 440 admissions to secondary care in England every year for assessment and treatment of carbon monoxide poisoning (National Institute for Health and Care Excellence(space)(NICE) Clinical Knowledge Summaries (CKS), 2023). Nearly 51% of admissions in England and Wales are because of accidental exposure to carbon monoxide, which, in residential settings, is most commonly a result of faulty piped gas appliances and the use of oil, gas or kerosene heaters without proper ventilation (such as poorly maintained gas boilers) (NICE CKS, 2023).
Indoor releases of carbon monoxide are commonly from oil, gas or kerosene heaters and faulty gas appliances (UK Health Security Agency (UKHSA), 2022). Other sources of carbon monoxide include open or enclosed fires (wood or coal-fuelled fires in the home) and accidental fires (including house fires). This correlates to the fact that nearly 50% of all mortality from unintentional non-fire related carbon monoxide poisoning in England and Wales between 1998 and 2019, occurred in the two most socioeconomically deprived quintiles (one-fifth) of the population (UKHSA, 2022). The current cost of living crisis is likely to have exacerbated this problem, particularly as the cost of maintaining equipment in good working order has increased. A worrying statistic was reported in a recent survey of gas engineers, where 45% of the participants observed an increase in the use of dangerous gas appliances in homes since the beginning of the cost of living crisis (ProjectSHOUT, 2024).
Nurses working in the community need adequate knowledge and skills to assess carbon monoxide risk within service users’ homes to ensure the safety of patients and healthcare professionals. This article will facilitate this aim by covering the following objectives:
- Revise human respiratory anatomy and physiology
- Discover how carbon monoxide interacts with human respiratory physiology
- Identify the symptoms of carbon monoxide poisoning
- Consider the emergency actions and treatments required after carbon monoxide exposure
- Identify the role of the community nurse in home safety, managing risk and the prevention of carbon monoxide poisoning.
Revision of respiratory physiology
The key function of the respiratory system is to distribute oxygen to the tissues, enabling the cells to produce energy through aerobic respiration and to remove waste products, primarily carbon dioxide. The human respiratory tract is divided into the upper respiratory tract (including the nose, pharynx and larynx) and the lower respiratory tract (including the trachea, bronchi, bronchioles, alveolar tract and alveoli). Using negative pressure produced by the respiratory muscles and diaphragm, environmental air is inhaled through the upper and lower respiratory tracts to reach the terminal alveoli, where gas exchange can occur. Similarly, waste gases are excreted back into the environment through a reverse process (Powers and Dhamoon, 2023).
Gas exchange is the process where oxygen and carbon dioxide move between the blood stream and the lungs. Gas exchange happens in the alveoli of the lungs and the blood of the pulmonary capillaries. For effective gas exchange, the alveoli must be both effectively ventilated and perfused. This involves a process of diffusion where molecules are driven by a concentration gradient, moving from an area of high concentration to an area of low concentration through a membrane (Nursing Fundamentals, 2021).
After diffusing into the pulmonary capillaries, 98% of the oxygen molecules bind to the haemoglobin contained within the red blood cells and 2% of oxygen dissolves within the blood plasma. Each haemoglobin molecule can carry 4 molecules of oxygen at which point it is ‘saturated’ (referred to as oxyhaemoglobin). When oxyhaemoglobin reaches tissues with oxygen requirement, it is released from the haemoglobin (Powers and Dhamoon, 2023). Similarly, carbon dioxide is the key waste product of cellular energy production and it is returned to the pulmonary system dissolved in plasma, attached to water molecules and bound to haemoglobin; this molecule is called deoxyhaemoglobin (Nursing Fundamentals, 2021).
Carbon monoxide: the chemistry
Carbon monoxide is a colourless, odourless and tasteless gas. It is released into the environment as a result of incomplete combustion of hydrocarbons, substances that contains carbon such as wood, gas, coal and oil. (Manaker and Perry, 2024). Carbon monoxide is the second most common polluting gas found in the lower layers of the atmosphere, despite significant reduction in industrial emission since 1990 (UKHSA, 2022). Exposure to carbon monoxide in the environment results in the gas entering the body through the lungs (Figure 1).
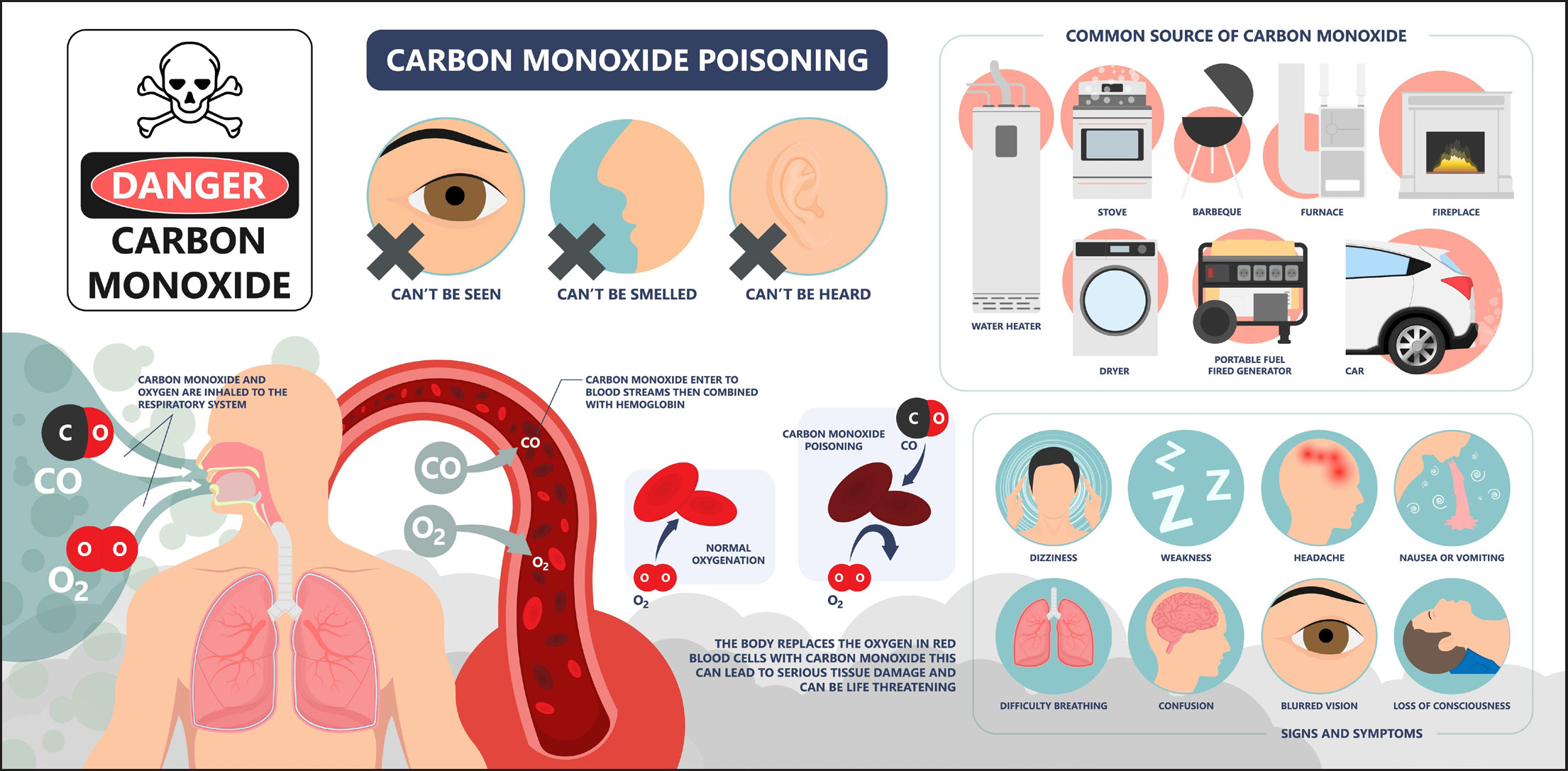
Carbon monoxide has strong ability to bind with haemoglobin molecules, creating carboxyhaemoglobin. In fact, carbon monoxide has a 220% greater binding affinity with haemoglobin than oxygen (Hanley and Patel, 2023). This means that when carbon monoxide and oxygen are diffused into the blood via gas exchange, carbon monoxide will bind to the available haemoglobin molecules, preventing oxygen from binding. This reduces the oxygen carrying ability of each affected haemoglobin molecule and will inevitably lead to cellular hypoxia (Manaker and Perry, 2024). Carboxyhaemoglobin further exacerbates tissue hypoxia because it increases the haemoglobin's affinity for oxygen. As a result, the unaffected oxyhaemoglobin does not release oxygen to the tissues (often described as a leftward shift of the oxygen dissociation curve) (Manaker and Perry, 2024). Sources of carbon monoxide include:
- Blocked or poorly maintained chimneys or flues
- Portable heaters using liquid petroleum gas or paraffin
- Gas boilers and gas appliances
- Gas cookers or clay ovens
- Car engines and generators
- Barbeque (charcoal or gas)
- Wood or coal burners (London Fire Brigade, 2019).
Symptoms
There is variation in the symptoms and symptom severity exhibited by patients with carbon monoxide poisoning. In general, it is accepted that there is a correlation between the severity of symptoms and percentage concentration of carboxyhaemoglobin. Table 1 presents the symptoms based on carboxyhaemoglobin levels. Cherry red skin and mucus membranes are not common signs of poisoning, and are normally only seen with higher levels of carboxyhaemoglobin (Manaker and Perry, 2024).
| Carboxyhaemoglobin level | Symptoms |
|---|---|
| 1−3% | Normal levels in a non-smoker |
| 4−9% | Smokers and some urban commuters |
| 15−20% | Mild signs of toxicity:
|
| 20−40% | Moderate or severe signs of toxicity:
|
| 40−60% | Extreme signs of toxicity:
|
| >60% | Can be fatal in minutes |
Adapted from: Open Anaesthesia (2015)
It is important to understand the pathophysiology of this process as it underpins why these symptoms manifest at different stages of carbon monoxide poisoning. As carboxyhaemoglobin levels rise within the blood stream, it results in capillary leakage from the systemic vasculature that can lead to cerebral oedema (Hanley and Patel, 2023). Simultaneously, cerebral blood vessels dilate and there is increased coronary blood flow (Open Anaesthesia, 2015).
At higher concentrations, carboxyhaemoglobin results in central respiratory depression, which leads to cerebral and coronary hypoxia (Welsh Government, 2015). Cardiac effects, including dysrhythmias, are common at this stage and are associated with mortality risk in this patient group, although there is evidence that myocardial dysfunction commences in the presence of low levels of carboxyhaemoglobin (approximately 20%) (Hanley and Patel, 2023).
Diagnosis
There are three common methods of carbon monoxide poisoning diagnosis.
- Carbon monoxide can be measured in expired air. Breath analysers are commonly used in smoking cessation and may provide useful clinical data in relation to diagnosis, but they are poor indicators of prognosis
- CO-oximetry probes (using a similar technique as oxygen saturation probes) can provide a useful measure of CO saturations in affected patients
- Blood tests can be sent to a laboratory or point-of-care testing can be undertaken locally (Welsh Government, 2015).
Diagnosing carbon monoxide poisoning without oximetry or blood tests can be difficult. It is recognised that these are unlikely to be available to community nurses as the equipment and point-of-care testing is not routinely available outside of the clinical setting. There are some suggested features which might help individuals identify potential carbon monoxide poisoning:
- Multiple persons with symptoms in the same house
- Symptoms improving after leaving the contaminated environment (when going out shopping)
- Symptoms becoming worse when using, or after using, a gas stove for cooking
- Symptoms becoming worse when using central heating, gas, oil or kerosine heater or an open fire (Welsh Government, 2015).
Emergency treatment
Treatment for carbon monoxide poisoning is mainly supportive and it is important that professionals call for help early on. Unwell individuals should be assessed using the airway, breathing, circulation, disability, exposure (ABCDE) approach and, if required, resuscitation should be attempted (Hammett, 2021). Many treatments including oxygen therapy may be outside the scope of practice of many nurses working in the community setting. Where oxygen therapy is available, it should begin without delay at the highest flow rate. A face mask should be used to deliver the highest concentration of oxygen possible (Open Anaesthesia, 2015).
The most important step is removing oneself and, where possible, the patient from the source of the exposure. This will normally involve moving outside. If this is not possible (eg the patient is bed bound), then it is important to open all the windows to ensure maximum ventilation as soon as possible and call for help. If a healthcare professional suspects ongoing exposure to carbon monoxide within the environment, it may be essential to leave the environment and wait for the emergency services to arrive. If possible, turn off gas appliances before leaving the property, but do not delay leaving the premises (London Fire Brigade, 2019).
Help from the emergency services is key to accessing definitive medical care and accurate information about potential carbon monoxide poisoning and the number of people possibly affected At an emergency department, the affected individuals can receive a formal diagnosis and definitive treatment. This includes oxygen therapy and, in the most severe cases, hyperbaric oxygen treatment. The source of the carbon monoxide should be found and fixed before an individual returns to the house or environment (Open Anaesthesia, 2015). For advice on poisonings, search TOXBASE (www.toxbase.org) or contact the National Poisons Information Service (NPIS) on 0844 892 0111.
Long-term effects on health and wellbeing
Carbon monoxide poisoning is associated with a high risk of mortality and long-term morbidity for those who survive the poisoning episode. Carbon monoxide poisoning can lead to long-term neurological problems similar to other anoxic brain injuries. This can affect memory, language use, cognition, movement and behaviour (Headway, 2024).
Safety in the home
It is important that health and social care professionals working in service users’ homes feel confident in identifying the risks of carbon monoxide contamination in the environment and providing health advice to service users. This should be included in local risk assessments. Indicative signs of potential carbon monoxide contamination include:
- Black, yellow or brown stains on or around a combustion appliance (gas cooker, heater or boiler)
- Smoke or excessive condensation accumulating in rooms because of poor ventilation and faulty flues
- Yellow or orange flames (instead of blue or violet flames) on gas appliances or boiler pilot lights
- Pilot lights frequently going out
- Unfamiliar or burning smell when gas or oil appliances are running (Welsh Government, 2015; London Fire Brigade, 2019).
It is important to advise service users to fit carbon monoxide alarms in all rooms that contain fuel burning appliances. The London Fire Brigade (2019) has the following advice for carbon monoxide alarms, which should be included in education for service users:
- Purchase an alarm from a reputable vendor
- Ensure that it has been certified to British Standard EN50291 and that it includes an approval mark, such as a kite mark
- Alarms should be fixed in any room that has a fuel burning appliance.
In England, it is a legal requirement for landlords to install a carbon monoxide alarm in any room that holds a solid fuel burning appliance. It remains the tenant's responsibility to test and maintain the device in functioning order (London Fire Brigade, 2019).
Advice for clinical staff working in service users’ home
The All-Party Parliamentary Carbon Monoxide Group published tips for practitioners in 2023:
- Understand carbon monoxide poisoning symptoms
- Recognise the potential sources of carbon monoxide in the home environment
- Know what to do if a carbon monoxide alarm sounds or if you suspect exposure
- Save the gas emergency number on your phone (0800 111 999)
- Inform service users about carbon monoxide poisoning, the importance of installing carbon monoxide alarms and how to stay safe through regular servicing of appliances
- Have an evacuation plan for each service user in advance. The employer should support staff with this
- Report safety risks. If you see unsafe housing, always escalate this referral onwards
- Always consider your safety. Follow your local ‘lone worker’ policy carefully (Policy Connect, 2023).
The acronym COMA (Cohabitees, Outdoors, Maintenance, Alarm)can be used by nurses working in service users’ homes to help consider the potential for carbon monoxide poisoning (Table 2; Royal College of Nursing, 2022).
| COMA—component | Description |
|---|---|
| C: cohabitees | Are there other individuals living or working in the same environment who are experiencing the same or similar symptoms? |
| O: outdoors | Do the symptoms improve when those affected go outside for a sustained period? |
| M: maintenance | Have all the combustion devices (such as a boiler or gas or wood burning appliance) been serviced in the last year? |
| A: alarm | Is there a carbon monoxide alarm fitted in the house? Is it working and has it been activated recently? |
Royal College of Nursing, 2022
Conclusions
In the current climate of increasing fuel and housing poverty, the risk of carbon monoxide exposure and poisoning may increase. Health and social care workers are well placed and have an important role to play in the identification of risk for carbon monoxide exposure and education of service users. Carbon monoxide should also be included in pre-visit risk assessments. To achieve this, professionals need sufficient education to support their knowledge, skills, confidence, and competence in this area. This article provided key information for professionals caring for service users in their own homes, and employers need to support professionals to integrate and implement this into clinical practice.
Key points
- Carbon monoxide poisoning is a public health issue associated with risks of mortality and morbidity for the service users and the healthcare professionals working in the community setting
- Carbon monoxide is generated by the incomplete combustion of substances that contain carbon. It is an odourless, tasteless and colourless gas
- Carbon monoxide has a stronger affinity than oxygen for binding with haemoglobin, which results in cellular hypoxia
- Treatment in the community involves early oxygen therapy and transfer through emergency services to the emergency department for definitive care
- Community nurses are well positioned to identify risks of carbon monoxide exposure within service users’ homes and living environments
CPD reflective questions
- What are your specific learning needs in relation to understanding carbon monoxide poisoning?
- Using your existing knowledge, list the important stages of respiratory ventilation and gas exchange
- List the key symptoms of carbon monoxide poisoning. Consider what other diseases can cause these symptoms and reflect on the challenges this could present when trying to identify if a patient has been exposed to carbon monoxide
- From your experience, which environmental factors could increase the risk of carbon monoxide contamination in a service users’ home environment?
- Briefly reflect on how this article will impact on and influence your clinical practice as a community nurse


