Health and Social Care Partnerships (HSCPs) were established in 2015 following the Scottish government's legislation under the Public Bodies (Joint Working) (Scotland) Act 2014 (Scottish Government, 2014). This legislation required the integration of health and social care services, ensuring that these services worked collaboratively by law, made the best use of local resources and promoted a positive experience for service users, carers and families. East Dunbartonshire is one of six HSCPs within NHS Greater Glasgow and Clyde in the west of Scotland and one of the largest health authorities in Europe (NHS Greater Glasgow and Clyde, 2023).
East Dunbartonshire has a population of just over 109000, with a significantly higher proportion of adults aged over 75 years than their neighbouring council areas (Healthandcare.scot, 2023). National Records of Scotland confirm a 69.6% increase in the number of adults aged 75 and over in East Dunbartonshire in 2001–2021 (National Records of Scotland, 2023a). This contrasts with Scotland's national picture which showed a 32.7% increase in this age group over the same period (National Records of Scotland, 2023b). The consequences of this have been an increased demand for healthcare services, with older individuals often requiring more complex care because of multiple comorbidities and polypharmacy.
Responding to these challenges, a district nurse advanced nurse practitioner (DNANP) role was introduced into a district nursing service in East Dunbartonshire HSCP as a test of change. Early indications have influenced workforce planning to expand the DNANP service, with plans to appoint three DNANPs across East Dunbartonshire by April 2024. This article describes the learning gained from the development, implementation and initial evaluation of the role.
Background
The historic district nursing service model embedded throughout NHS Greater Glasgow and Clyde comprises a specialist practitioner district nurse, community staff nurses and healthcare support workers with team sizes determined by the aligned GP practice population size and demographics. The increasing demands and complexity placed on district nursing services have been widely explored, with the Queen's Nursing Institute (QNI) proposing potential solutions to ensure that workforce retention and role development are prioritised (QNI, 2022). The DNANP role was introduced in East Dunbartonshire in February 2021 with a single practitioner to explore the concept that an advanced practitioner role could support the transformation of the district nursing service, subsequently addressing the identified workforce pressures.
At the outset, key outcomes were aligned with the chief nursing officer for Scotland's vision for transforming district nursing roles (Scottish Government, 2017a) and with East Dunbartonshire HSCP's strategic priorities related to palliative care, frailty and unscheduled care. Transforming District Nursing Roles (Paper 3) addressed the priorities of shifting care from hospital to home by using innovative approaches in the provision of safe, effective and person-centred care within district nursing services (Scottish Government, 2017a). This publication is part of a series of papers focused on the transformation of Scotland's nursing, midwifery and allied health care professional roles, enabling patients to receive care in their preferred place while preventing avoidable hospital admissions through integrated team approaches (Scottish Government, 2017b).
Educational preparation
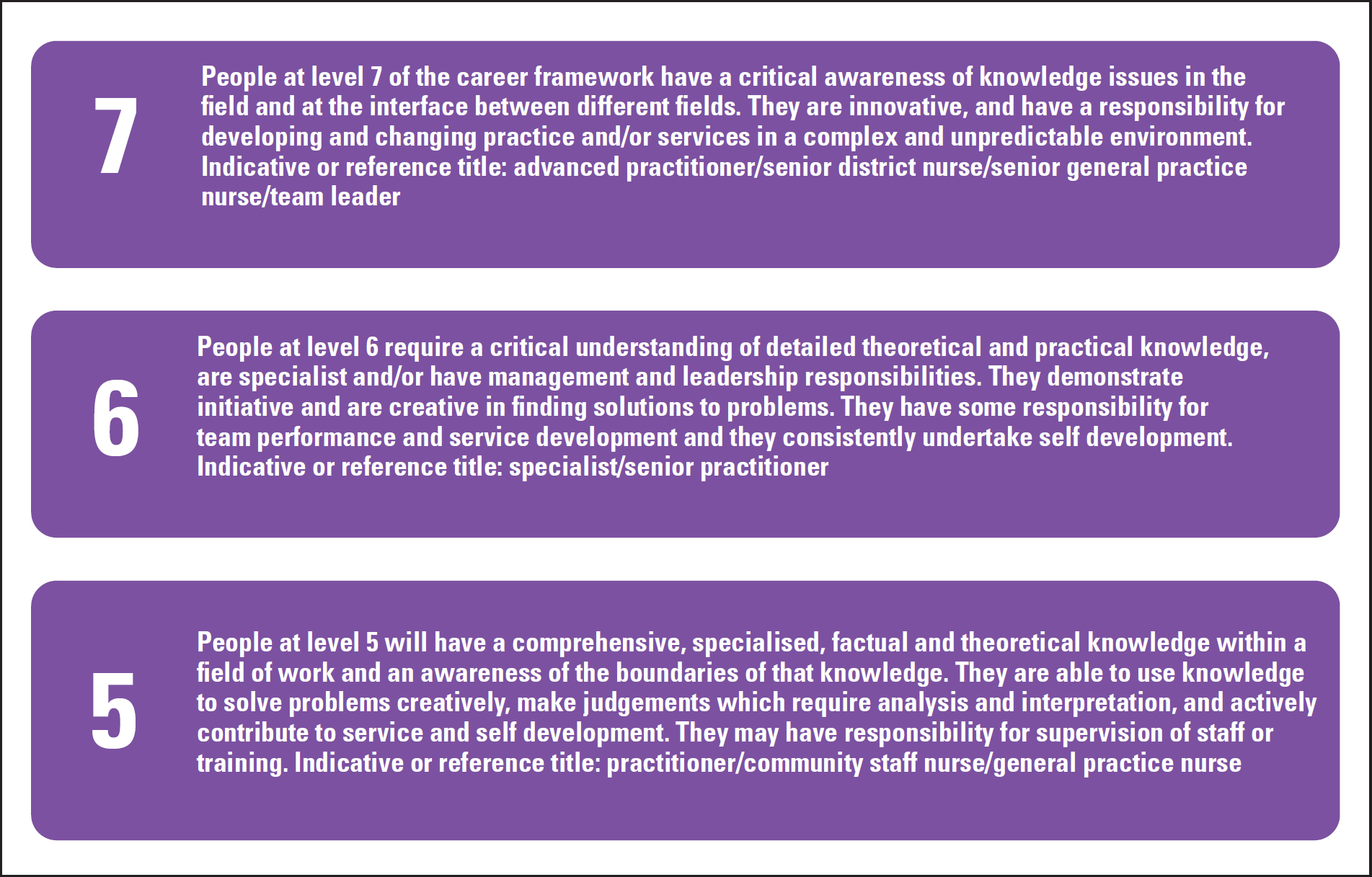
A DNANP is a qualified advanced nurse practitioner with a Nursing and Midwifery Council recorded specialist practitioner qualification and is also registered on the Scottish Workforce Information Standard System (SWISS) for advanced nurse practitioners. Insisting on this essential criterion develops an attractive career pathway that also retains the expert knowledge and experience of the district nurse within the service. This approach has fostered professional respect and effective partnership working between established district nurses and the pioneering DNANP role, while clearly demonstrating the distinction between level 6 and level 7 practice (Figure 1). In February 2022, East Dunbartonshire progressed with the appointment of the second DNANP post in the HSCP, with the successful candidate being a level 6 practitioner appointed from the local district nursing service. Reflecting on the training and development requirements of the existing DNANP, a robust model of clinical supervision and education was developed to meet the prerequisites for entry onto the SWISS register.
Modules in advanced research methods, advanced clinical assessment and independent prescribing, which were part of the district nursing post-graduate diploma, are also included as core modules in the advancing professional practice educational pathway. As a result, the trainee DNANP was required to complete two additional Master's level academic modules and submit a comprehensive professional portfolio of evidence to support the requirements of the NHS Greater Glasgow and Clyde advanced nurse practitioner final sign-off process (NHS Greater Glasgow and Clyde, 2022). The training model developed was focused on ensuring the DNANP was equipped with the knowledge, competence and experience needed to deliver on the service priorities of transforming the district nursing service, while fostering the development of a competent and autonomous leader.
Clinical practice
The DNANP is accountable and responsible for the complete and autonomous assessment, treatment, appropriate referral and follow-up of patients with undifferentiated diagnoses and complex presentations. East Dunbartonshire HSCP can confidently demonstrate a shift in demand, with fewer GP house calls and hospital conveyances and more complex care being exclusively managed within core health and social care teams surrounding the DNANP.
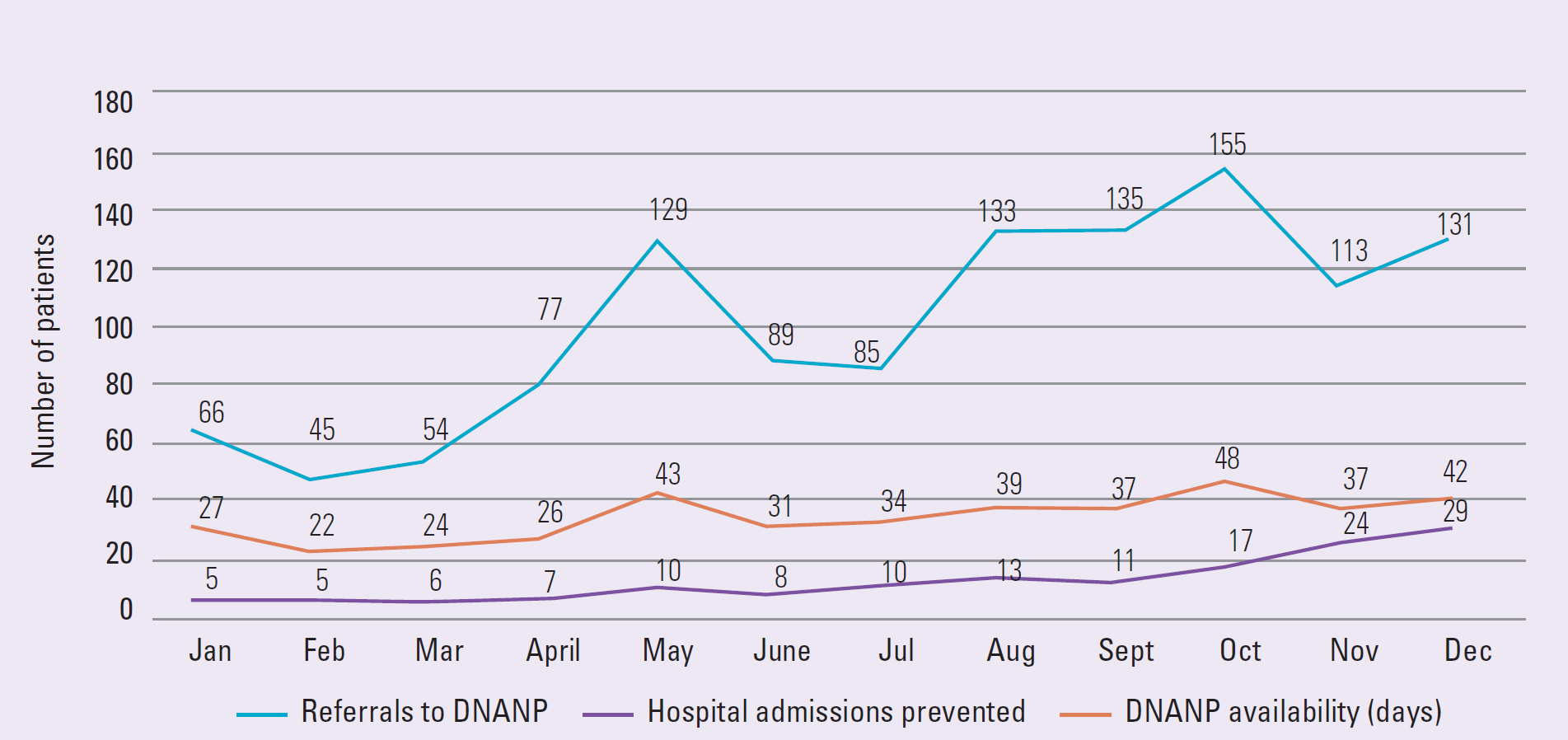
Referrals to the DNANP are received from all members of the district nursing team for patients presenting with acute, undifferentiated diagnoses or deterioration in their long-term conditions. This referral process marked a departure from historical ways of working, where the district nuring team escalated all clinical concerns to the patient's GP, a service already under significant pressure. Figure 2 illustrates the increasing referral rates, which have steadily risen in line with growing confidence in the DNANP's competency.
The increasing number of referrals to the DNANP has been accompanied by a steady improvement in the quality of clinical information provided by the district nursing staff and an increase in complexity; an indication of the team's improved identification of a deteriorating patient. Evaluation of district nursing practices before the introduction of the DNANP revealed a reliance on intuition or clinical judgment alone when concerns arose about a patient's wellbeing. Clinical observations of patients were rarely considered before district nursing staff requested a GP house call, which risked delays in treatment or inappropriate escalation to the GP.
At the outset, the DNANP service prioritised focusing on the recognition of deterioration, basic assessment skills and referral processes. Recognising the need for robust identification of deterioration and a reliable escalation process is essential to safeguard patient safety and ensure appropriate hospital conveyance (Health Improvement Scotland, 2023).
Health Improvement Scotland (2023) asserts that improved patient outcomes depend on healthcare systems meeting the demands of their local populations by creating appropriate escalation processes operated by capable and suitably trained clinical staff. The creation of the DNANP role within district nursing teams ensured that East Dunbartonshire HSCP adhered to the principles of the national guideline SIGN 167 Care of Deteriorating Patients (Health Improvement Scotland, 2023).
The availability of the DNANP during the out-of-hours period in East Dunbartonshire increased from 50% to 100% of all weekends starting in September 2023. The DNANP completed an average of four face-to-face consultations per day, covering an area of approximately 109 square miles and was available from 09:00 to 17:00 on Saturdays and Sundays.
Additionally, the DNANP provided clinical advice and prescribing support to district nursing staff, all of which would typically have resulted in an out-of-hours GP referral. Scrutiny of all face-to-face consultations undertaken during this period, including peak times of winter pressures, provided valuable insights into the wide range of presentations assessed and managed by a single advanced practitioner during the out-of-hours period (Figure 3). The greatest number of requests were for complex symptoms experienced at the end of a patient's life. Respiratory, urology, gastrointestinal and dermatology presentations were also common referrals, including acute infections, bowel obstructions, acute exacerbations of long-term conditions and red flag symptoms requiring urgent suspicion of cancer referrals (NHS Scotland, 2022).

Medical emergencies such as sepsis, acute kidney injuries, head injuries and chest pain were assessed and managed autonomously by the DNANP. This ensured that patients on a district nursing caseload in East Dunbartonshire had access to a reliable escalation process during the out-of-hours period, managed by suitably trained clinicians who delivered appropriate care to deteriorating patients at the right time.
Lessons learned from the DNANP audit were shared throughout NHS Greater Glasgow and Clyde, and have supported East Dunbartonshire's workforce planning to ensure better preparation for periods of increased demand, including winter pressures.
Facilitation of learning
DNANP's maximise the role of the district nurse by promoting and supporting advanced clinical assessment skills and independent prescribing practices within an appropriate scope of practice. Strategies developed by the DNANP to achieve this include providing a practice assessor role during district nursing specialist practitioner qualification training, complemented by regular advanced clinical supervision, coaching and governance for all qualified district nurses. The limited use of advanced assessment and non-medical prescribing skills by district nurses is well-documented, with competence and confidence often cited as self-identified barriers to appropriately using these skills (Downer and Shepherd, 2010).
East Dunbartonshire's approach is showing transformation, with a noticeable increase in the appropriate use of district nursing advanced assessment and prescribing practices since the introduction of the DNANP. Experienced district nurses with V300 qualifications have acknowledged that their previous prescribing practices were limited to dressings, catheter supplies and first-line palliative care drugs. However, they now feel more confident and competent in prescribing for patients presenting with conditions such as catheter-associated urinary tract infections, wound infections, lower respiratory tract infections and more complex palliative care issues, including complex pain and opioid toxicity.
The advanced level of knowledge, practice and leadership required of the DNANP enables them to contribute significantly to the facilitation of learning and development within the district nursing team, ranging from healthcare support workers to district nursing caseload holders. The existing DNANP team collaborates to create and deliver learning resources, addressing recognised pressures within the service and identified gaps in knowledge.
In 2024, the DNANPs facilitated a problem-focused supervision session for Level 5 and 6 district nursing staff in East Dunbartonshire. It focused on common gastrointestinal presentations, offering a masterclass on constipation, gastroenteritis and red flag symptoms. This session improved the identification and appropriate management of gastrointestinal conditions, while promoting patient safety at the same time.
Leadership
The leadership accomplishments of this advanced practice role were recognised at the inaugural Royal College of Nursing (RCN) Scotland Nurse of the Year awards, where East Dunbartonshire's first DNANP (MD) was awarded the clinical leadership award for her ‘courageous and ambitious approach to the development of the DNANP role and service’ (RCN, 2023). Public Health Scotland highlights the need for a whole-systems approach to collaborative leadership in addressing health inequalities, emphasising essential skills such as understanding the system, political awareness, meaningful collaboration, influencing change, leading change and innovation (Public Health Scotland, 2021). The DNANP has played a key leadership role in this context within the HSCP, particularly in the planning and implementation of work streams targeting national and local priorities, including the prevention of avoidable hospital admissions through effective future care planning (Scottish Government, 2023).
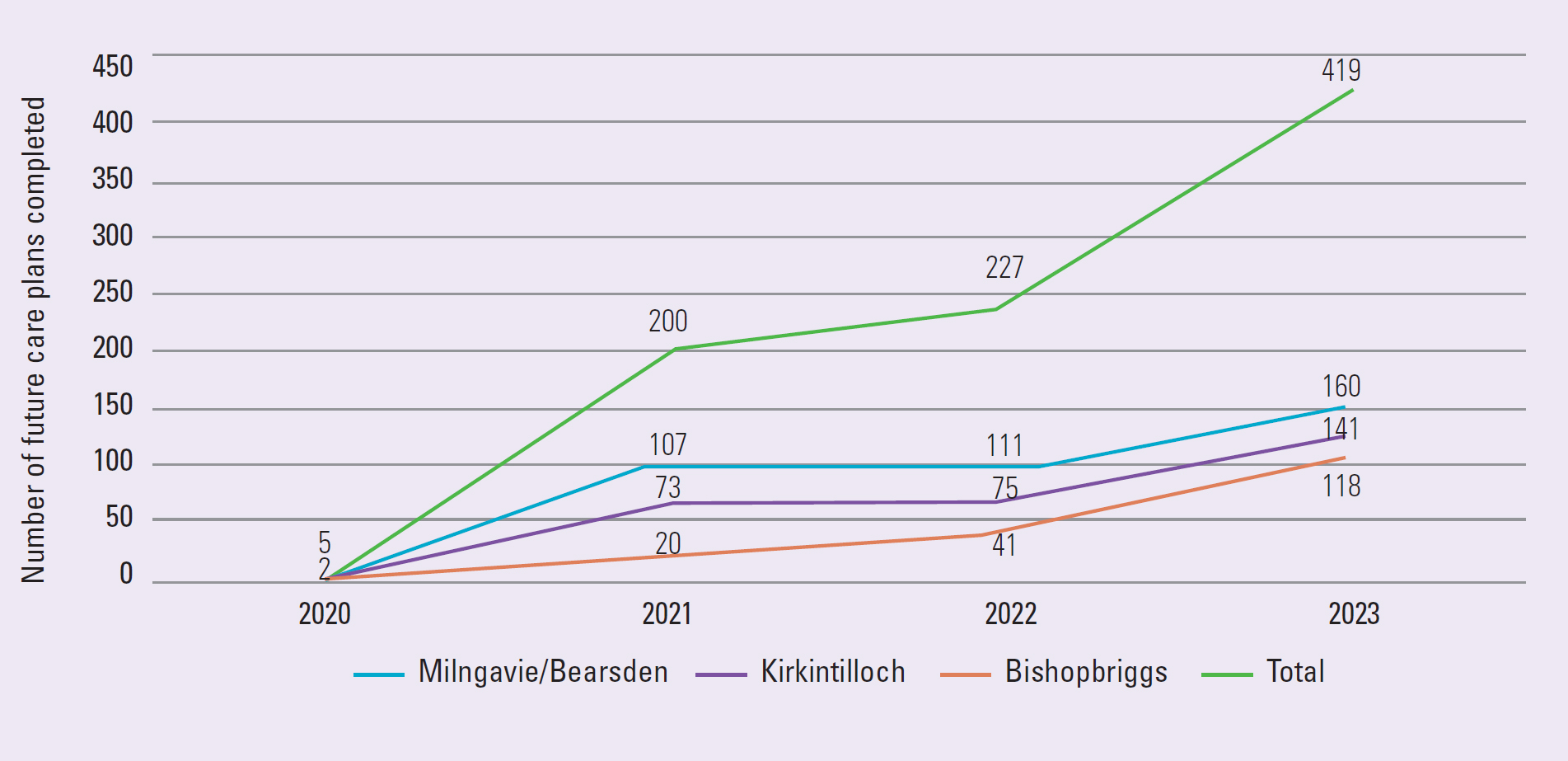
As the lead for East Dunbartonshire's future care planning workstream, the DNANP (appointed in 2021) engaged all local service leads through a steering group, fostering the development of future care planning champions across adult health and social care services. Data from NHS Greater Glasgow and Clyde's business intelligence confirms a yearly increase in the number of future care plans recorded for East Dunbartonshire residents, rising from 5 in 2020 to 629 in 2023. This growth is significantly higher than in neighbouring HSCPs, with a direct correlation between the introduction of a DNANP and the increase in anticipatory care planning across the three areas (Figure 4). The evidence supports the view that the presence of a DNANP within a DN team enhances role development, drives change and ensures quality assurance across the system.
Evidence, research and service development
Ensuring the provision of evidence-based practice across district nursing services, the DNANP has led service development through an innovative approach to quality improvement. By identifying appropriate quality outcome measures—such as improving patient outcomes and reducing avoidable hospital admissions through enhanced future care planning—the DNANP developed a data collection tool to gather relevant quality information. This data, collected and analysed by the DNANP since the service's implementation, has informed this evaluation as well as innovations within the wider adult community nursing services.
Embedded within the DNANP's scope of practice is the provision of complex palliative and end-of-life care. The number and complexity of patients requiring palliative care have increased, reflecting the added pressures on the NHS since the onset of the COVID-19 pandemic (Savinc and Atherton, 2023). The study confirms a 35% increase in deaths at home since the start of the pandemic, the majority of which were not COVID-19-related, with rates not returning to pre-pandemic levels.
Retrospective analysis of data collected in the Milngavie/Bearsden locality where the first DNANP was appointed shows a sharp increase in the number of deaths at home for all patients with known palliative care needs on a district nursing caseload. This increase is believed to be linked to improved future care planning and the advanced level of care provided by the DNANP (Figure 5).
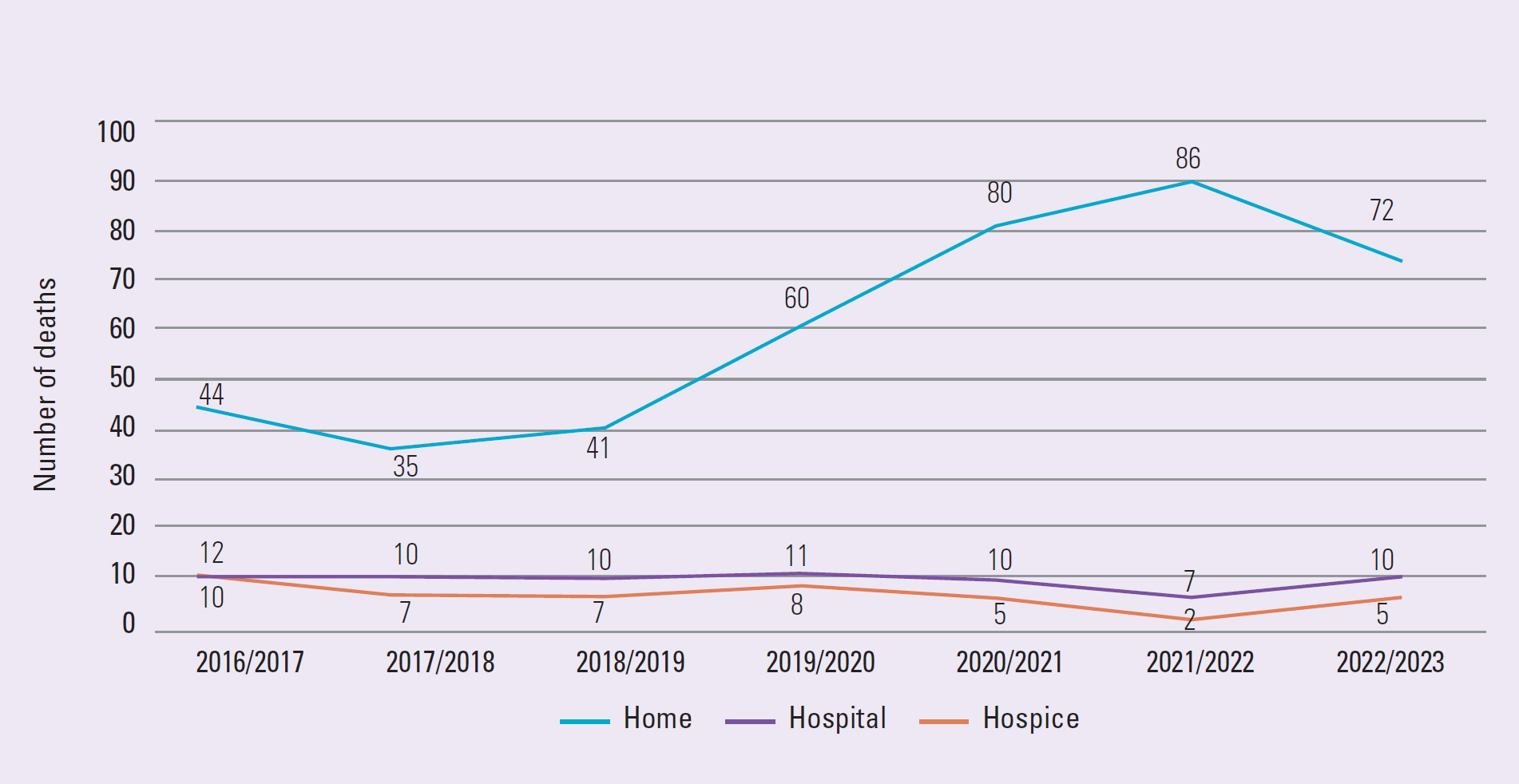
An exploration of local palliative care services in East Dunbartonshire since the onset of the COVID-19 pandemic, reveals a change in the service delivery model for specialist palliative care provision for patients in their own home. Enhancing collaborative palliative care services was identified as a priority during the first 6 months in post, with the availability of the DNANP during the out-of-hours period and improved collaboration with specialist palliative care services suggested as possible solutions to supporting patients with complex palliative care needs to remain at home.
Reflecting on the provision of palliative care since the introduction of the DNANP in East Dunbartonshire highlights the benefits of partnership working with local hospices. This collaboration has enabled the delivery of the highest standards of palliative care during both in-hours and out-of-hours periods, supporting patients with complex needs to achieve optimal symptom control and remain in their preferred place of care.
Discussion
By transforming the district nursing service in East Dunbartonshire through the introduction of an advanced practice role, the HSCP has created an appealing career pathway for level 6 district nurses. Feedback from service users, carers and their families has been overwhelmingly positive, with responses highlighting that care was delivered promptly, led by service users and alleviated the burden of navigating multiple services and professionals.
In contrast to some other nationally prescribed models of advanced practice, East Dunbartonshire HSCP's model has required minimal additional investment to enhance core services year-round. This approach is expected to reduce pressure on other parts of the wider healthcare system, particularly GPs, both in and out of hours, while also helping to decrease avoidable hospital admissions.
Conclusions
Evaluation of the data collected by the DNANP since its implementation has shown that this role is crucial in leading a whole-systems approach to improving patient outcomes while supporting the transformation of district nursing roles. This service development has facilitated a shift in care from hospital to community services by empowering district nurses to work within their scope of practice and delivering a timely response to escalation requests, ensuring the right care is provided at the right time and in the right place.
By applying advanced-level knowledge, gained through extensive academic qualifications and post-registration experience, the DNANP role demonstrates the skills and expertise needed to transform district nursing services and deliver high standards of complex, evidence-based care to patients in a home setting. Further research into the role is needed to develop a nationally recognised DNANP job description to ensure standardisation and prevent gross inconsistencies in the application of the DNANP role.


